-
Health & Wellness
Mayo Clinic Q and A: Causes of fecal incontinence vary, but treatment is available
DEAR MAYO CLINIC: What causes fecal incontinence? Can it be treated?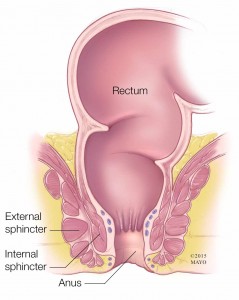
ANSWER: Fecal incontinence, or leakage of stool from the rectum, can range from occasional leakage while passing gas to a complete loss of bowel control. An estimated 8 percent of the general population and 15 percent of people age 70 and older are affected. Although fecal incontinence is more common in middle-aged and older adults, it isn’t an inevitable part of aging. It’s often the result of another treatable medical issue or can be a warning sign of a more serious problem.
Your rectum and anus are at the end of your large intestine. Normally, the muscles and nerves in and around these two structures sense the presence of waste, allow storage in the rectum, and then move and eliminate stool. Changes in the function of this complex system can interfere with normal stool elimination.
Damage to these muscles or nerves are potential causes of fecal incontinence. It may be difficult to hold stool back if muscles at the end of the rectum are damaged during childbirth, or hemorrhoid or cancer surgery. Weak or improperly functioning pelvic floor muscles (which support the organs in the lower abdomen and pelvis) also can contribute to fecal incontinence, as can injury to nerves that sense stool in the rectum or that control the anal sphincters. Childbirth, a habit of straining to pass stool, a spinal cord injury, a stroke and even certain diseases (such as diabetes and multiple sclerosis) can affect these nerves.
Chronic constipation or diarrhea also can result in fecal incontinence. Ongoing constipation can lead to a hard, dry stool in the rectum that’s too hard to pass. As a result, muscles in the rectum and intestines stretch, weakening and allowing watery stool from farther up to leak out around the hard mass. It can also cause nerves in the anus and rectum to become less responsive to the presence of stool. Diarrhea can cause or make fecal incontinence worse, since it’s easier to retain solid stool in the rectum than loose stool.
In addition, changes in the rectum wall that cause the rectum to stiffen (from radiation treatment, rectal surgery or inflammatory bowel disease) may reduce its capacity to hold stool.
Once fecal incontinence is diagnosed and the likely cause is identified, your doctor can discuss treatment options that may be best suited to your situation. It’s not unusual to use multiple approaches to treat fecal incontinence.
What you eat and drink affects stool consistency and how fast it passes through your digestive system. If constipation is causing fecal incontinence, your doctor may recommend drinking plenty of fluids and gradually increasing your intake of fiber-rich foods. Getting adequate fiber can help with diarrhea, too. Avoid beverages with caffeine, alcohol, milk and carbonation if they trigger diarrhea. Artificial sweeteners and high fructose corn syrup also can produce diarrhea.
Sometimes, medications you’re taking for other conditions can contribute to fecal incontinence. If that’s the case, your doctor can make appropriate medication changes to help reduce aggravation of fecal incontinence. It’s important that your doctor is aware of all prescription and nonprescription drugs and supplements you’re taking.
Other possible treatments may include pelvic floor exercises, biofeedback, and bowel training (determining a specific time of day to have a bowel movement). A relatively new treatment —electrical stimulation of the sacral nerves — may be considered if more conservative measures aren’t successful.
Surgical treatments for fecal incontinence may be necessary when the cause is related to pelvic floor damage or muscle injuries that affect the anal sphincter. Surgery also may be done to repair protrusion of the rectum through the anus (rectal prolapse) or through the vagina (rectocele), or for hemorrhoids that interfere with bowel function. If damage to the anal sphincter is severe, a new sphincter may be constructed.
Don’t shy away from talking to your doctor about fecal incontinence. Better understanding of the disorder, awareness, and improvements in diagnosis and treatment make it possible for many people with the condition to be helped. — Stephanie L. Hansel, M.D., Gastroenterology, Mayo Clinic, Rochester, Minn. (adapted from Mayo Clinic Health Letter)
Related Articles







