-
Mayo Clinic Q and A: COPD treatment with two types of bronchodilators
 DEAR MAYO CLINIC: I was recently diagnosed with chronic obstructive pulmonary disease (COPD). Why do I have different inhalers?
DEAR MAYO CLINIC: I was recently diagnosed with chronic obstructive pulmonary disease (COPD). Why do I have different inhalers?
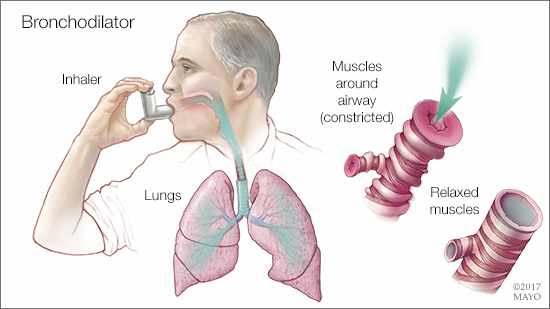
ANSWER: Bronchodilators commonly are prescribed for people with COPD. Bronchodilators relax the muscles around your airways so that you can breathe better. They usually come in the form of an inhaler, which allows the medicine quick access to your lungs as you breathe it in. Two of the most commonly used classes of bronchodilators are beta agonists and anticholinergics.
Some bronchodilators offer quick relief. These are called short-acting bronchodilators. They typically start working in 15 to 30 minutes, and last about four to six hours. Your doctor may prescribe a short-acting bronchodilator if your COPD is mild and you only have symptoms every once in a while. Examples of short-acting bronchodilators are albuterol (ProAir HFA, Ventolin HFA, and other brand names), levalbuterol (Xopenex) and ipratropium (Atrovent HFA).
Most long-acting bronchodilators don’t act as quickly but last longer — 12 to 24 hours or more — to relieve symptoms. Long-acting bronchodilators usually are prescribed when symptoms occur frequently. These medications act as maintenance therapy by keeping symptoms from developing in the first place. Most are not as good at providing immediate relief. Examples of long-acting bronchodilators are formoterol (Foradil, Perforomist), salmeterol (Serevent), and tiotropium (Spiriva), and there are numerous others.
If your COPD is moderate to severe, your doctor likely will recommend both types — a short-acting bronchodilator for quick relief when needed and one or more long-acting ones that you take every day to keep symptoms at bay. Consider labeling each with a marker, so you can quickly tell which is for quick relief and which is for regular treatment.
Some people with COPD are prone to frequent exacerbations, or flare-ups, of symptoms, which may require the use of antibiotics or steroids, or both. A number of medications help reduce the risk of exacerbations, including both classes of long-acting bronchodilators, as well as inhaled corticosteroids, an antibiotic (azithromycin), and roflumilast (Daliresp).
If you have frequent exacerbations despite daily use of a long-acting bronchodilator, talk to your doctor. A combination with additional medicines may work better for you. (adapted from Mayo Clinic Health Letter) — Dr. Paul Scanlon, Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota
Related Articles