-
Mayo Clinic Q and A: Diagnosing ovarian cancer
 DEAR MAYO CLINIC: Why is ovarian cancer almost always diagnosed when it’s already late-stage? Are there any tests that can help health care providers detect ovarian cancer earlier? Who’s at risk for this disease?
DEAR MAYO CLINIC: Why is ovarian cancer almost always diagnosed when it’s already late-stage? Are there any tests that can help health care providers detect ovarian cancer earlier? Who’s at risk for this disease?
ANSWER: Ovarian cancer is hard to detect in its early stages, because symptoms are usually either nonexistent or they are vague. Unfortunately, by the time symptoms become more obvious, the disease often has spread beyond the ovaries. There are no screening tests for ovarian cancer. A number of factors, including genetics, can raise a woman’s risk for the disease.
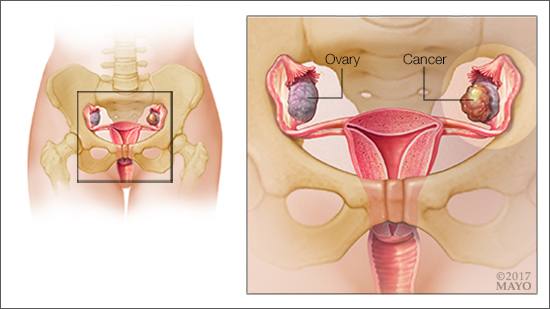
Women have two ovaries — one on each side of the uterus. They produce eggs, along with the hormones estrogen and progesterone. When cancer starts in the ovaries, it rarely causes any symptoms. The ovaries are so small and located so deep within the pelvis that the cancer has to grow significantly before it causes any symptoms.
When symptoms develop, they are often nonspecific. Symptoms may include constipation or diarrhea, bloating, feeling full quickly when you eat, back pain, shortness of breath, or chest pain. In addition, exam findings, such as a distended abdomen, a pelvic mass or decreased breath sounds in the lungs, may raise the suspicion of ovarian cancer.
If ovarian cancer is suspected based on symptoms or exam, women often will undergo a CT scan of the abdomen and pelvis, or an ultrasound of the pelvis. On a CT scan, a health care provider may see an ovarian mass, tumors within the abdomen or extra fluid within the abdomen — all of which would increase the suspicion of ovarian cancer. A blood test, CA 125, also is often used to help guide health care providers to an ovarian cancer diagnosis.
A diagnosis of ovarian cancer can be made only through pathology with tumor biopsy or removal. Ovarian cancer is categorized by its stage, which is usually determined during surgery. In stage 1, the cancer is contained within the ovaries. In stage 2, the cancer has moved beyond the ovaries but is still within the pelvis. Stage 3 means ovarian cancer has spread to the abdomen. With stage 4, the cancer has spread to the liver or organs outside of the abdomen.
It’s typical for women to be diagnosed with ovarian cancer initially at stage 3. At that point, it is challenging to treat and, unfortunately, the disease is frequently fatal. More than 14,000 women die every year from ovarian cancer.
While there is no good screening test to check for ovarian cancer, for women at high risk of developing the disease, a health care provider may recommend some tests in an effort to catch ovarian cancer early. They include an ultrasound of the pelvis and a blood test that can detect a protein called CA125 that’s found on the surface of ovarian cancer cells.
Factors that may increase a woman’s risk for ovarian cancer include smoking, endometriosis, a family history of ovarian cancer, infertility, having a history of polycystic ovary disease, never being pregnant, and obesity. Women who started their periods before age 12 or who went through menopause after age 52 also appear to be at higher risk. Age may play a role, too, as ovarian cancer is most common in women between the ages of 50 and 60.
A small number of ovarian cancers cases are caused by a genetic mutation. The genes known to increase the risk of ovarian cancer are called breast cancer gene 1, or BRCA1, and breast cancer gene 2, or BRCA2. Originally, these genes were identified in families with multiple cases of breast cancer, which is how they got their names. But women with these mutations also have a significantly increased risk of ovarian cancer. The gene mutations that cause Lynch syndrome — an inherited condition associated with colon cancer — also raise a woman’s risk of ovarian cancer.
If you are concerned about your risk for ovarian cancer, talk to your health care provider. He or she can review your medical and family history with you to see if you may be at high risk, and if so, help you decide on the best strategy moving forward. — Dr. Carrie Langstraat, Medical Oncology, Mayo Clinic, Rochester, Minnesota







