 DEAR MAYO CLINIC: After my last colonoscopy, I was told I have diverticulosis. Will this lead to diverticulitis? I currently have no symptoms but wonder if I should do anything to prevent it from progressing.
DEAR MAYO CLINIC: After my last colonoscopy, I was told I have diverticulosis. Will this lead to diverticulitis? I currently have no symptoms but wonder if I should do anything to prevent it from progressing.
ANSWER: Although the two conditions are related, and diverticulosis is a risk factor for diverticulitis, many people who have diverticulosis never go on to have diverticulitis. In those who do eventually develop diverticulitis, it is not clear what causes the condition, so it’s difficult to know how to prevent it. A healthy diet and regular exercise may help.
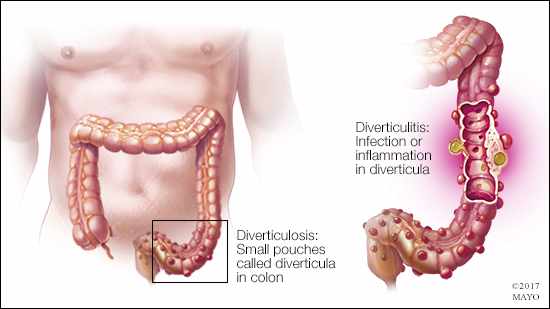
Diverticulosis is a condition that affects the gastrointestinal tract. Small sacs, called diverticula, bulge out of the wall of your colon. The condition is very common as people age. Estimates are that about half of the U.S. population over 50 has diverticulosis. Most people have it by the time they reach 80. With those statistics in mind, a finding of diverticulosis during a colonoscopy isn’t unusual. Generally, it’s not a cause for concern.
Diverticulosis by itself typically doesn’t trigger any symptoms. Rarely, diverticula may bleed, causing blood in the stool. As in your case, diverticulosis is often found during a routine colonoscopy or on an imaging exam, such as a CT scan, that’s done for another reason. You can have diverticulosis for years without any complications or problems. If one or more of the diverticula become inflamed, however, that condition is diverticulitis.
While diverticulosis usually doesn’t lead to any discomfort, diverticulitis can be quite painful. Common symptoms include significant abdominal pain, as well as fever, constipation or diarrhea, nausea, and fatigue. A mild case of diverticulitis may go away on its own without any treatment. When treatment is necessary, antibiotics and a liquid or low-fiber diet may be all that is necessary to resolve symptoms.
However, in more severe cases, diverticulitis can lead to a tear in the colon that allows bowel contents to leak into the abdomen. In that situation, hospitalization usually is required for effective treatment. In some cases, emergency surgery may be necessary to repair a hole in the colon.
In contrast to diverticulosis, diverticulitis is uncommon. Only about 5 percent of people who have diverticulosis ever go on to develop diverticulitis. In general, diverticulitis is poorly understood. Unfortunately, little is known about what leads a person with diverticulosis to develop diverticulitis.
Although limited knowledge about what causes diverticulitis makes it difficult to offer solid prevention strategies, there are a few guidelines that may help. People who are overweight tend to develop diverticulitis more often that people who are at a healthy weight. So, exercising regularly and maintaining a healthy weight may provide some protective benefit against diverticulitis. Some research suggests diet also may play a role, with people who eat a low-fiber diet possibly at increased risk for diverticulitis. Eating a well-balanced diet that includes plenty of fiber may prevent diverticulitis.
If you have questions or concerns about diverticulosis, talk to your health care provider. He or she may be able to offer suggestions based on your individual medical situation. If you experience symptoms that could be related to diverticulitis — especially sudden pain in your abdomen — seek medical care right away. — Dr. David Etzioni, Colon and Rectal Surgery, Mayo Clinic, Scottsdale, Arizona







