-
Health & Wellness
Mayo Clinic Q and A: Endometrial ablation when pelvic pain or endometriosis are present
DEAR MAYO CLINIC: I've been diagnosed with endometriosis and have heavy menstrual bleeding. My health care provider said I should consider endometrial ablation. A friend told me it might be problematic because I'm only in my late 20s, and it could affect my ability to conceive a child down the road. What are the risks? Are other treatments available?
ANSWER: Endometrial ablation can reduce heavy menstrual bleeding significantly. But you should consider the potential risks associated with this procedure, especially if you are suspected to have endometriosis based on pelvic pain.
Women are sometimes given a diagnosis of endometriosis based on symptoms, including pelvic pain and heavy periods, but definitive diagnosis is only possible with biopsy or excision of lesions — usually performed laparoscopically. This is called a keyhole surgery. If endometriosis is confirmed with surgery, then the recommendation for treatment is excision of the endometriosis.
Alternatives to surgery for endometriosis can include hormonal suppression with pills, an intrauterine device, subdermal implants or injections. While endometriosis has no cure, these treatments can reduce symptoms to a more manageable level in some cases. It is important to realize that surgical removal of endometriosis will not necessarily help with heavy menstrual bleeding.
During your period, your body sheds the lining of your uterus, called the "endometrium." When periods become unusually heavy on a regular basis, the condition should be evaluated. In general, producing enough blood to soak through a pad or tampon every two hours or less is considered heavy flow. Heavy menstrual bleeding often is treated initially with hormonal suppression, as discussed above. But it also can be treated with endometrial ablation, as mentioned by your health care provider.
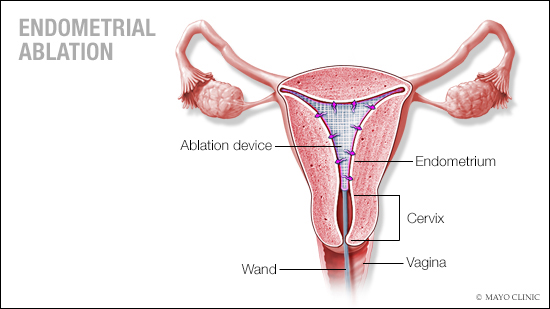
Endometrial ablation destroys the uterine lining. Although techniques vary, the procedure usually is conducted using instruments that deliver heat or extreme cold to the endometrium. After endometrial ablation, many women still have periods, but they are much lighter.
Age is a major factor in how likely you are to experience problems after endometrial ablation. Age plays a role in that trend because ablation techniques rarely destroy all of the endometrium, and the endometrium has a tendency to regenerate prior to menopause. The younger a patient is when she has endometrial ablation, the longer the endometrium has to grow back and the more opportunities there are for complications to arise over the years.
When age is the only consideration, research shows that the ideal ablation candidate generally is older than 40. Due to the risk of uterine cancer after menopause, endometrial ablation is typically not recommended after menopause.
One consequence of endometrial ablation is that scar tissue forms within the uterus after the procedure, changing the structure of the uterine cavity. Because of that change, if you have abnormal bleeding after endometrial ablation it can be more challenging for your health care provider to assess the cause of the bleeding and treat it. The scar tissue also can obstruct menstrual flow. In some cases, that causes pain.
If abnormal bleeding or persistent pain presents after endometrial ablation, surgical removal of the uterus — a hysterectomy — may be necessary. Multiple studies have looked at predictors to determine which women are most likely to require a hysterectomy after endometrial ablation. Although many predictors have been reported, the most consistent is age. Research shows endometrial ablation gives predictable results for the first five to seven years following the procedure. Rates of hysterectomy trend upward after that.
In one Mayo Clinic study of women who had endometrial ablation, factors that increased the risk of requiring a hysterectomy after ablation included being younger than 45 at the time of ablation, significant menstrual pain before ablation, and tubal ligation before ablation. If a woman had all three risk factors, there was a 50% to 60% chance of hysterectomy within five years of ablation. Conversely, in patients older than 45 without significant menstrual pain before the procedure and no history of tubal ligation, only about 5% required a hysterectomy within five years of ablation.
Given your age and potential pregnancy plans, endometrial ablation would not be recommended. Pregnancies following endometrial ablation are high-risk for both the mother and her baby.
For younger women like yourself, other effective treatments outside of ablation are available to ease heavy menstrual bleeding, including hormonal medications, birth control pills and intrauterine devices. Discuss all your options, along with their risks and benefits, with your health care provider to decide which choice is best for you. — Dr. Christopher Destephano, Obstetrics and Gynecology, Mayo Clinic, Jacksonville, Florida
****************************
Related Articles
- Consumer Health: Endometriosis, ovarian cancer and infertility — what are the connections? published 5/10/21
- Women’s Wellness: Learn about endometriosis published 10/17/19
Related Articles







