-
Cardiovascular
Mayo Clinic Q and A: Evaluating and treating leg numbness and cramping
 DEAR MAYO CLINIC: I have been on medication to treat peripheral artery disease for nearly a year, but it doesn’t seem to help the numbness and cramping in my legs. Are stents always effective in treating symptoms of peripheral artery disease, or is there a chance I’ll still have symptoms even with stents?
DEAR MAYO CLINIC: I have been on medication to treat peripheral artery disease for nearly a year, but it doesn’t seem to help the numbness and cramping in my legs. Are stents always effective in treating symptoms of peripheral artery disease, or is there a chance I’ll still have symptoms even with stents?
ANSWER: Your leg numbness and cramping could be connected to peripheral artery disease. Or they could be related to something else. Tell your doctor about your symptoms, and ask for an evaluation to confirm their source. If peripheral artery disease is the cause, look into additional treatment. That treatment could include a procedure to open the arteries, such as stenting. But other options are available, too.
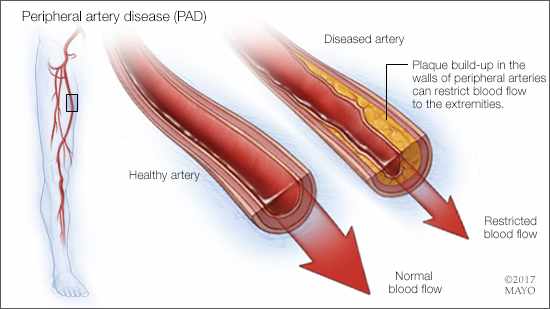
Peripheral artery disease affects the arteries that supply oxygen and nutrients to your leg muscles. Peripheral artery disease happens when plaque builds up in those arteries, narrowing them and sometimes blocking them completely. When arteries are narrowed or blocked, the oxygen and nutrients in your blood can’t get to your tissues and muscles easily.
Leg cramping when you walk is a hallmark symptom of peripheral artery disease. It usually goes away within a few minutes after you stop walking. Other symptoms may include leg numbness, tightness or weakness when you walk. Atypical leg symptoms, such as leg fatigue, may be more common symptoms in peripheral artery disease than classic cramping-type symptoms.
Medication to relieve symptoms is often a first-line treatment for peripheral artery disease. For example, the drug cilostazol may be prescribed, as it improves the distance people with peripheral artery disease can walk without leg symptoms. Medication to control underlying medical conditions that can contribute to peripheral artery disease, such as high cholesterol, high blood pressure and high blood sugar, also may ease symptoms.
Lifestyle changes are an important part of peripheral artery disease treatment, too. Smoking contributes to constriction and damage of your arteries, and can make peripheral artery disease worse. If you smoke, quitting is the most important thing you can do to reduce your risk of peripheral artery disease complications. Regular exercise also is crucial. Exercise helps your body use oxygen more efficiently and conditions your muscles. Both may reduce peripheral artery disease symptoms.
If managing underlying medical conditions, taking medication to relieve peripheral artery disease symptoms and lifestyle changes aren’t enough to keep symptoms in check, then it’s time to reassess your condition. It’s possible your numbness and cramping could be the result of a different medical problem, such as a disorder related to your veins or a condition affecting your nerves. These symptoms also can be side effects of certain medications. Ask your doctor to review your current medications to see if this is a possibility for you.
If an assessment of your condition suggests peripheral artery disease is the cause of persistent leg numbness and cramping, then you may want to consider a procedure to open the arteries in your legs. The specific procedure used depends on the level, extent and type of blockage. In some cases, a stent — a small mesh framework — is placed in an artery to keep it open. A small balloon also can be inflated within an artery to reopen it and flatten the blockage against the artery wall. Another alternative is to remove the plaque using a procedure called atherectomy.
In severe cases of peripheral artery disease, your doctor may recommend a procedure to bypass the artery affected by peripheral artery disease. A graft bypass created using a blood vessel from another part of your body or using a blood vessel made of synthetic fabric can be placed in your leg. That allows the blood to flow around the blocked or narrowed artery. In many cases, artery-opening procedures reduce or eliminate peripheral artery disease symptoms. But it is possible some symptoms may linger after this treatment.
Make an appointment to talk with your doctor about your symptoms, and have them evaluated. If they are related to peripheral artery disease, it’s likely that additional treatment and lifestyle changes can help with your symptoms and, if not resolve them completely, reduce them to a point that they are manageable. — Dr. Shahyar Gharacholou, Cardiovascular Diseases, Mayo Clinic, Jacksonville, Florida







