-
Featured News
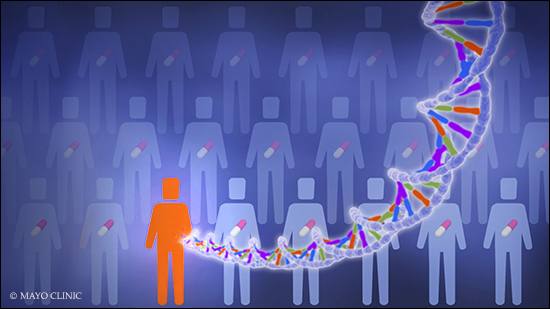
Mayo Clinic Q and A: Genetic testing and antidepressants
DEAR MAYO CLINIC: I’ve heard that genetic testing can help determine which antidepressant would be best for me. How does this work?
ANSWER: Genetic testing is available to help narrow down your antidepressant options, ideally reducing the need for a sometimes prolonged trial-and-error period while settling on an antidepressant regimen. Although these tests can’t tell you specifically which antidepressant would work best to treat your depression, they offer clues about how your body may respond.
This testing — known as pharmacogenomics — looks for changes or variations in genes that determine how quickly a drug is processed, or metabolized, in your body or whether you might have side effects from a certain drug.
Pharmacogenomic tests check your DNA — obtained by a blood draw or a swab for saliva — for genes that encode certain enzymes, and the results can be classified according to how fast your body metabolizes and gets rid of certain medications, such as particular antidepressants. For example, if testing indicates that your body metabolizes a drug too slowly, the drug might build up in your body and increase the likelihood of side effects. While the drug still may be useful for you, lower doses may be appropriate. On the other hand, if testing suggests that the drug would leave your body quickly, it may not have a chance to work properly or would require a dose that is larger than normal.
However, genetic testing has limits. Most of these tests focus on how your body metabolizes a drug rather than on how the drug influences the cause of disease — although some tests address that issue, as well. Cost is also an issue, as not all insurance companies cover this type of testing.
Choosing antidepressants based on your health history and symptoms is still the standard that health care providers use when prescribing these medications. Routine genetic testing isn’t recommended at this time. Still, the testing may offer important clues to aid in drug selection and dosing, especially for people having trouble finding an effective option with few side effects. (adapted from Mayo Clinic Health Letter) — Dr. Richard Weinshilboum, Pharmacology, Mayo Clinic, Rochester, Minnesota
****************************
Related Articles
- Mayo Clinic Minute: The differences between adult and teen depression published 9/10/19
- Mayo Clinic Q and A: New treatment for hard-to-treat depression published 7/12/19
- Mayo Clinic Minute: How esketamine can help severe depression published 5/7/19
- Mayo Clinic Q and A: Depression in older adults published 5/3/19
- Housecall: Genetic testing — is it right for you? published 4/22/19
- New Mayo Clinic GeneGuide DNA testing application provides genetic testing, insights backed by Mayo Clinic expertise published 10/1/18
- Science Saturday: Direct to consumer genetic testing shifting landscape published 2/10/18
- Mayo Clinic Q and A: Pharmacogenomics — individualizing medication to improve care published 1/19/18
- Mayo Clinic Minute: 3 things to know about home genetic testing published 10/4/17







