-
Cardiovascular
Mayo Clinic Q and A: Heart attack symptoms in women
 DEAR MAYO CLINIC: Is it true that women have different symptoms of a heart attack than men? If so, why does this happen, and what are the symptoms in women?
DEAR MAYO CLINIC: Is it true that women have different symptoms of a heart attack than men? If so, why does this happen, and what are the symptoms in women?
ANSWER: Heart attack symptoms in women can be similar to those in men, but there are some crucial differences. Women’s symptoms tend to be more subtle and may be more ambiguous. Along with being able to recognize possible heart attack symptoms, as a woman, it’s also important to understand your own personal risk factors for heart disease and to get help right away if you suspect a heart attack.
Although it may not be the first disorder that comes to mind when you think of women’s health issues, heart disease is the leading cause of death in both women and men in the U.S. And a 2016 research study found that women die more often than men from heart disease.
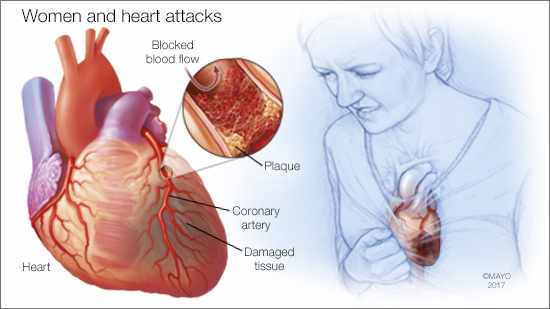
With those sobering statistics in mind, the importance of knowing what to look for when it comes to a heart attack can’t be overstated. Many are familiar with the hallmark symptoms of a heart attack: crushing chest pain, pain radiating down one arm, nausea and vomiting. Women who have a heart attack may experience all of these symptoms. But they are often less obvious than when they happen in men.
For example, chest pain is a common heart attack symptom in women, but it’s often not the predominant symptom or the only symptom. Women’s chest pain usually is not as severe as men’s chest pain. Often the chest pain may be accompanied by other symptoms, such as shortness of breath, fatigue and nausea. In addition, the pain may not be just in the chest, but in the back, shoulder or neck, too.
There’s no clear explanation for why heart attack symptoms appear differently in women than they do in men. A few factors may play a role. In women, heart disease tends to affect the smaller cardiac vessels more often than in men. Tight artery blockages are not as common in women as in men. Women’s vessels sometimes are smaller, and the vessel walls often are stiffer in women. But whether these factors are the underlying cause of the variation in symptoms between men and women is not well-understood.
What is known is that many of the risk factors for heart disease are the same for women and men. Diabetes, smoking, high blood pressure, high cholesterol, being overweight, lack of regular physical activity, and an unhealthy diet all raise the risk for heart disease. It’s important to note, too, that some of these factors play a bigger role in the development of heart disease in women. A woman who smokes is at greater risk for heart disease than a man who smokes, as is a woman who has diabetes.
There also are some specific risk factors that affect only females. Women who have high blood pressure during pregnancy — a condition called preeclampsia — are at increased risk later in life for heart disease. After menopause, when estrogen levels drop, the rate of heart disease in women goes up dramatically.
Take time to talk with your health care provider about your individual risks for heart disease. Review your personal and family medical history, so you can better understand your risk overall. If you think you might be having a heart attack — even if the symptoms seem vague — don’t ignore them, and don’t wait. Get emergency help right away. Don’t drive yourself to the hospital. Call 911. — Dr. Rekha Mankad, Cardiovascular Diseases, Mayo Clinic, Rochester, Minnesota







