DEAR MAYO CLINIC: I know COVID-19 has been around now for over a year, but I'm still confused by the different types of vaccines, including messenger RNA and vector vaccines. Can you explain how these vaccines work and the differences between these vaccines?
ANSWER: COVID-19 vaccines can help you develop immunity to SARS-CoV-2, the virus that causes COVID-19, without getting ill. But how the different types of COVID-19 vaccines work is a question many people ask.
Vaccines prompt an immune response so that your body remembers how to fight a virus in the future. Some vaccines use a whole virus to cause your immune system to respond. Other vaccines use parts of the virus or genetic material that provides instructions for making specific proteins like those in the virus.
Many COVID-19 vaccines involve a spikelike structure on the surface of the COVID-19 virus called an S protein. The S protein helps the virus get inside your cells and start an infection.
Manufacturers around the world are working on different types of vaccines. The main types of COVID-19 vaccines available in the U.S. or in large-scale clinical trials are:
- Messenger RNA vaccine
This type of vaccine uses genetically engineered messenger RNA to instruct your cells how to make a harmless piece of the S protein found on the surface of the COVID-19 virus. After vaccination, your immune cells begin making the S protein pieces and displaying them on cell surfaces. This causes your body to create antibodies. If you become infected with the COVID-19 virus, these antibodies will fight the virus. After the messenger RNA vaccine helps your cells make the protein pieces, the messenger RNA is immediately broken down. It never enters the nucleus of your cells, where your DNA is kept. Both the Moderna and Pfizer COVID-19 vaccines use messenger RNA.
- Vector vaccine
In this type of vaccine, genetic material from the COVID-19 virus is inserted into a different kind of weakened live virus, such as an adenovirus. The weakened virus, or viral vector, serves as a delivery system. When the viral vector gets into your cells, it delivers genetic material from the COVID-19 virus that gives your cells instructions to make copies of the S protein. Once your cells display the S proteins on their surfaces, your immune system responds by creating antibodies and defensive white blood cells. If you become infected with the COVID-19 virus, the antibodies will fight the virus. Viral vector vaccines can't cause you to become infected with the COVID-19 virus or the viral vector virus. Also, the genetic material that's delivered doesn't become part of your DNA. The Johnson & Johnson (J&J) and AstraZeneca COVID-19 vaccines are vector vaccines.
- Protein subunit vaccine
Subunit vaccines include only the parts of a virus that best stimulate your immune system. This type of COVID-19 vaccine contains harmless S proteins. Once your immune system recognizes the S proteins, it creates antibodies and defensive white blood cells. If you become infected with the COVID-19 virus, the antibodies will fight the virus. Novavax is working on a protein subunit COVID-19 vaccine.
The Food and Drug Administration (FDA) has granted emergency use authorization for the J&J, Moderna and Pfizer COVID-19 vaccines. the AstraZeneca COVID-19 vaccine has not yet been granted emergency use authorization.
The FDA and the Centers for Disease Control and Prevention have recommended that use of the J&J vaccine continue in the U.S. because the benefits outweigh the risks. If you are given this vaccine, you should be educated about the possible risks and symptoms of a blood clotting problem.
More types of COVID-19 vaccines are expected to be authorized for use over the coming months.
Being vaccinated for COVID-19 might prevent you from getting COVID-19, or from becoming seriously ill or dying due to COVID-19. Consult your local health department for the latest information on how and when you can receive a vaccine. — Compiled by Mayo Clinic Staff
____________________________________________
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
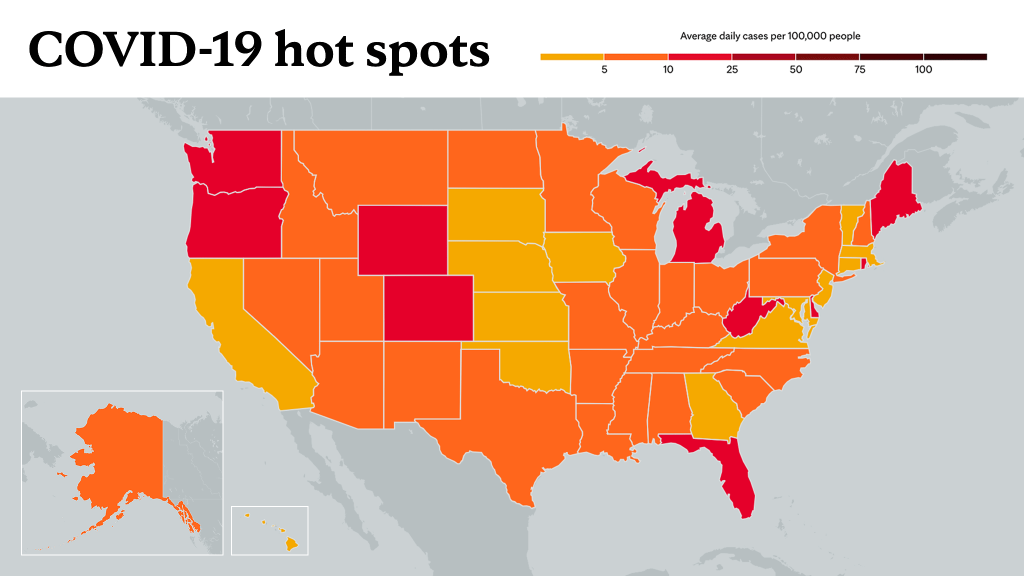
Learn more about tracking COVID-19 and COVID-19 trends.