
DEAR MAYO CLINIC: What would cause someone to become lactose-intolerant later in life? I’m in my 40s and have never had an issue with dairy, but, now, I can’t seem to have it without problems. Do I need to see a doctor to be tested for allergies, or should I just avoid dairy?
ANSWER: Lactose intolerance isn’t a true allergy, and it can develop at any age. In some people, lactose intolerance may be triggered by another medical condition, such as Crohn’s disease. In others, it develops without a specific underlying cause. It would be a good idea to have your condition evaluated by your doctor to confirm that what you’re dealing with truly is lactose intolerance.
Lactose intolerance results from a problem with the carbohydrate lactose, a type of sugar found in dairy products. When you eat or drink dairy products, enzymes in your small intestine digest lactose, so the body can make energy. In people with lactose intolerance, a certain enzyme, called lactase, is missing from the body. When those people eat dairy products, the body has no way to break down the lactose. This leads to fermentation of the sugar in the intestines and triggers symptoms, such as diarrhea, nausea, abdominal cramps, bloating and gas.
Sometimes, lactose intolerance develops when the small intestine’s production of lactase decreases after an illness, injury or surgery involving the small intestine. This is called secondary lactose intolerance. Among the diseases associated with this kind of lactose intolerance are celiac disease, bacterial overgrowth and Crohn’s disease. Treatment of the underlying disorder may restore lactase levels and improve symptoms.
More common than secondary lactose intolerance is primary lactose intolerance. People who develop primary lactose intolerance start life making normal levels of lactase — a necessity for infants, who get all their nutrition from milk. As children replace milk with other foods, lactase production normally decreases. It stays high enough, though, to digest the amount of dairy in a typical adult diet. In primary lactose intolerance, lactase production declines below normal at some point for reasons that are unclear. The low amount of lactase then makes milk products difficult to digest and leads to lactose intolerance symptoms.
Your doctor can confirm a diagnosis of lactose intolerance with a clinical test. One that’s often used is a lactose tolerance test. It assesses your body’s reaction to a dose of lactose. After you consume a drink containing lactose, a sample of your blood is taken to measure glucose levels. If your glucose level does not rise, it means your body isn’t properly digesting and absorbing the lactose.
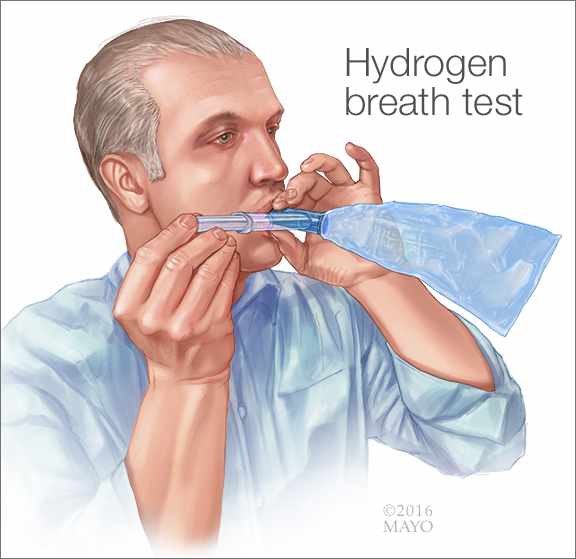
Alternatively, another test called the hydrogen breath test may be used. This test also requires you to consume a drink that contains high levels of lactose. Your doctor next measures the amount of hydrogen in your breath. Normally, very little hydrogen is detectable. However, if your body doesn’t digest the lactose, the fermentation reaction in your colon releases hydrogen and other gases. Your intestines absorb those gases, and you exhale them. Larger-than-normal amounts of hydrogen measured during this test are a sign that your body isn’t fully digesting and absorbing lactose.
If you have lactose intolerance, there isn’t a way to cure it. The most effective way for people with lactose intolerance to get relief from symptoms is to lower the amount of dairy products they eat. You may be able to use dairy products that have reduced levels of lactose or are lactose-free. Some people who have lactose intolerance benefit from taking lactase enzyme supplements, as well.
If test results do not point to lactose intolerance, your doctor may recommend additional tests to check for another condition that could be causing your symptoms, such as a milk allergy, intestinal disorders or other problems within your digestive tract. — Dr. Rohit Divekar, Allergic Diseases, Mayo Clinic, Rochester, Minnesota







