-
Health & Wellness
Mayo Clinic Q and A: Living liver donation
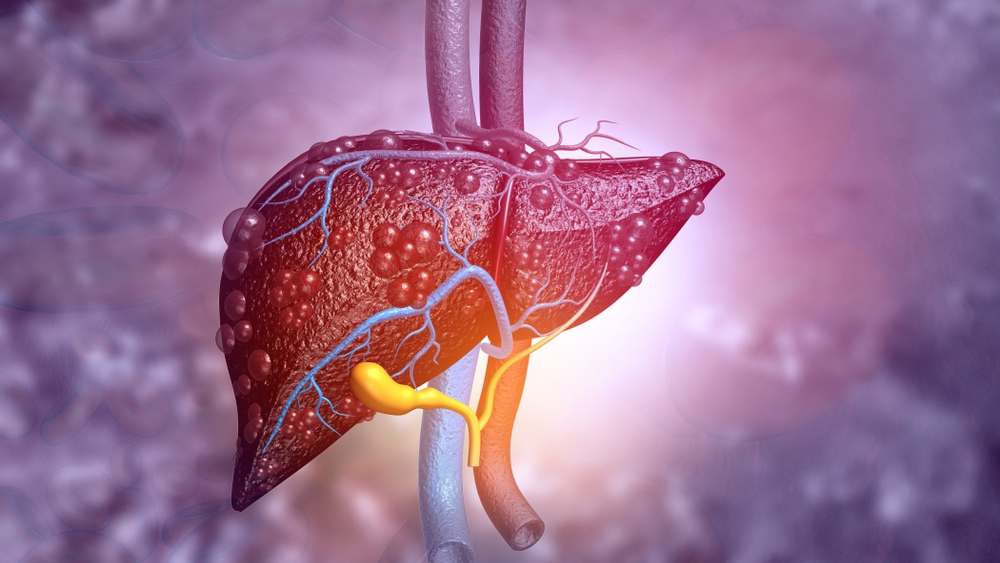
DEAR MAYO CLINIC: A colleague of mine recently shared the news that he was listed for a liver transplant. He then mentioned that he was hoping to find a suitable donor for a living liver transplant. I thought organ donors had to be deceased. Can you explain living liver donation and who is eligible?
ANSWER: More than 100,000 people in the U.S. are on the national waiting list to receive a donor liver, kidney, lung, heart or pancreas for a transplant. Of those people, 12,000 to 13,000 people are waiting for a new liver. However, about 1 in 5 patients ― or approximately 2,500 people ― who are waiting for a liver transplant will die or become too sick before an organ becomes available.
Traditionally, most organ donations come from a deceased donor. However, there has been a growing role in transplants from living donations, specifically with kidneys and now with liver transplantation.
Over the past year, the number of living donor liver transplants has doubled, now accounting for about 6% of all liver transplants nationwide. A liver transplant from a living donor is a surgical procedure where a portion of the liver from a healthy living person is removed and placed into someone whose liver no longer works properly.
Many people are surprised to learn that the liver can regenerate itself. That is one reason why we are able to perform these transplants. Liver tissue regenerates in the donor and recipient. Up to 70% of the donor liver can be removed for transplantation, and the liver regenerates in the donor and recipient to nearly full-size in about three to four weeks. A donor does not have to be related to a patient to donate a liver.
Survival outcomes are generally similar for recipients who receive a liver from a living donor or from a deceased donor. Technical issues during a living liver surgery can be somewhat higher for the recipient because it's more difficult to transplant a partial organ. For instance, there can be increased risk of bile duct complications and arterial thromboses, which are blood clots that can develop in arteries. However, living donor liver transplants typically occur before the recipient becomes dangerously ill awaiting transplant. So the timing improves the outcome for the patient.
While living donors traditionally have been people who know the recipient, such as a family member or friend, it is not required. That said, potential liver donors must be in good physical health. Donors are usually under 60. People interested in donating undergo blood tests to determine if their blood and tissue types are compatible with the organ recipient.
While it is a significant operation for the donor, recent improvements have aided in recovery. In the past, the surgery required a larger incision, but over the past four years, a hybrid procedure has been used that reduces the size of the incision, and that translates into better pain control. The time in the hospital is about four to six days, and typically it takes about four to six weeks for donors to have a full recovery.
To address the ongoing shortage of organs for people in need of transplants, Mayo Clinic recently launched the Living Liver Non-Directed Program and the Liver Paired Donation Program. These two initiatives, which are a part of the William J. von Liebig Center for Transplantation and Clinical Regeneration at Mayo Clinic in Rochester, Minnesota, aim to improve the opportunities for patients in need of a liver transplant.
Until recently, Mayo Clinic only accepted directed living donations, meaning the donated part of the liver is intended for a person known by the donor. With the Living Liver Non-Directed Program, donations are now accepted from people who have no recipient in mind but want to offer the gift of life to another person.
Both programs have guidelines and procedures similar to Mayo's successful programs for living kidney donors.
With so many people in need of transplants, I always encourage people who wish to become an organ donor to make their wishes known to their family and take advantage of the opportunity to highlight that choice on your state-issued driver's license or identification card.
As far as becoming a living donor, if you have a desire to give to a family member or friend, or donate altruistically to a stranger, speak to your primary health care provider about next steps for a referral to an evaluation center. —Dr. Timucin Taner, Transplantation Surgery, Mayo Clinic, Rochester, Minnesota
****************************
Related Articles
- Mayo Clinic Q&A podcast: Mayo Clinic expands living liver donation program published 11/30/20
- Expert Alert: 5 things to know about being a living liver donor published 11/10/20
Related Articles







