-
Featured News
Mayo Clinic Q and A: Managing the symptoms of vaginal atrophy
 DEAR MAYO CLINIC: Which products or medications are best for lessening the dryness that occurs because of vaginal atrophy?
DEAR MAYO CLINIC: Which products or medications are best for lessening the dryness that occurs because of vaginal atrophy?
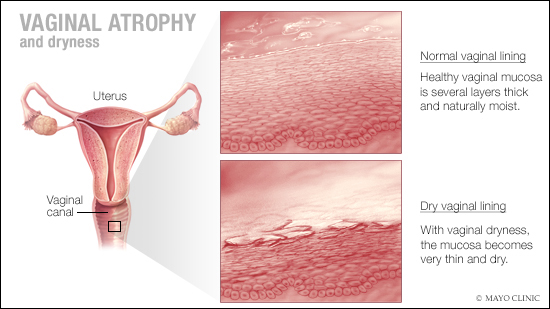
ANSWER: Vaginal atrophy — a thinning, drying and sometimes inflammation of the vaginal walls — is one of the most common challenges women face after menopause. It’s believed that atrophy of vaginal tissues affects up to half of these women. There are a number of things you can try to lessen your symptoms.
Vaginal atrophy occurs when the estrogen levels in your body drop, usually after menopause. The condition may make intercourse painful due to vaginal dryness or irritation, and decreased lubrication during sex. In addition, it often leads to distressing urinary symptoms, such as burning with urination, urinary urgency, incontinence and urinary tract infections. Hence, the newer term for vaginal atrophy is genitourinary syndrome of menopause.
Some women may begin to notice symptoms in the years leading up to menopause. Others may not experience a problem until several years into menopause. In addition to naturally occurring or surgically induced menopause, certain radiation therapies, anti-estrogen hormone therapies and chemotherapies for cancer also may affect estrogen levels enough to cause vaginal and urinary changes.
For women who experience vaginal dryness or irritation, there are actions and products that can help. First, try a vaginal moisturizer. Over-the-counter products such as K-Y LiquiBeads, Replens and Sliquid Naturals Satin can be used to restore moisture to the vaginal walls. These products are applied several times a week, usually at bedtime.
In addition, nonprescription hypoallergenic water- or silicone-based lubricants can improve discomfort from intercourse by reducing friction. Choose products that don’t contain glycerin or preservatives, since women who are sensitive to these substances may experience burning and irritation. Avoid products containing petroleum jelly, such as Vaseline.
If your symptoms are bothersome even after trying vaginal moisturizers and lubricants, don’t hesitate to talk to your health care provider about other options. In particular, vaginal estrogen therapy is the most effective treatment for moderate to severe atrophy symptoms. Vaginal estrogen therapy may come in the form of a cream, ring, tablet or softgel that’s inserted into the vagina.
Vaginal estrogen is formulated in a much lower dose, compared to systemic estrogen. Vaginally applied estrogen is readily absorbed by the local tissues, resulting in minimal absorption of estrogen in the bloodstream. This is particularly favorable in situations where systemic estrogen is likely to have a higher risk of side effects, as in women with a prior history of blood clots. Vaginal estrogen also can be used in some women with a previous history of breast cancer, but this is a complex decision that needs to involve a patient’s oncology team.
Systemic estrogen therapy delivered as a patch, gel or pill, or vaginal ring, is formulated to provide estrogen to the whole body. Due to the systemic exposure to estrogen with this route, it is not the preferred therapy if the only indication for estrogen is vaginal atrophy. However, systemic estrogen therapy can be used as first-line treatment in women experiencing hot flashes, night sweats and vaginal dryness at the same time.
Genitourinary syndrome of menopause can involve the urinary system and cause bladder urgency, urge incontinence and predisposition to recurrent urinary tract infections. Vaginal estrogen can relieve these symptoms and improve women’s quality of life. Some women also experience stress incontinence during menopause. Pelvic floor exercises, commonly known as Kegels, can strengthen the muscles that support the uterus and bladder, and may relieve symptoms of stress incontinence.
Advanced vaginal atrophy may lead to uncomfortable intercourse. If this occurs, talk to your health care provider. In addition to vaginal estrogen, lubricants and moisturizers, your provider may recommend additional treatments, including vaginal dilators and a referral to a pelvic floor physical therapist for the treatment of painful intercourse. If possible, maintaining a level of sexual activity is an effective way to optimize vaginal health, as it improves blood flow to the vagina and keeps the tissues more elastic. (adapted from Mayo Clinic Health Letter) — Dr. Richa Sood, Menopause and Women’s Sexual Health Clinic, Mayo Clinic, Rochester, Minnesota
****************************
Related Articles
- Women’s Wellness: Signs and symptoms of vaginal health problems published 6/21/18
- Stephanie Faubion, M.D., talks genitourinary syndrome of menopause published 12/1/17







