-
Mayo Clinic Q and A: Pregnancy and deep vein thrombosis
DEAR MAYO CLINIC: I’ve been a runner since high school but was diagnosed with deep vein thrombosis (DVT) during my first pregnancy, so stopped running for a few months. I am now nine weeks pregnant with my second baby and continue to run for exercise, but I’m worried I’ll develop DVT again. Should I be concerned?
ANSWER: Because you experienced a previous episode of DVT during a prior pregnancy, you are at an increased risk for DVT recurrence during the current pregnancy. Doctors typically recommend that women in your situation receive medication to help prevent blood clots throughout pregnancy. You do not necessarily need to stop running during pregnancy, but it would be a good idea to talk with your doctor to decide what’s best for your individual circumstances.
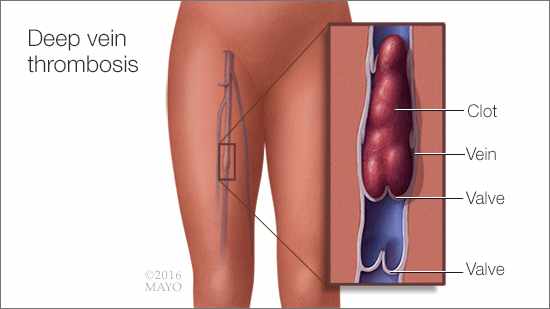
DVT happens when a blood clot forms in a vein typically located deep within the leg or pelvis. Clots can be caused by anything that prevents blood from circulating normally, as well as from the increased tendency to clot that accompanies pregnancy — a condition known as a hypercoagulable state. DVT is serious, because, if a clot in the leg or pelvis breaks free and travels to your lungs, it can be a life-threatening emergency (pulmonary embolus).
A variety of factors can increase your risk for DVT, including pregnancy. That’s because, when you are pregnant, the pressure in the veins in your pelvis and legs increases. Other factors that can increase DVT risk include a family history of DVT, certain genetic disorders (thrombophilias), obesity, immobility, surgery, hospitalization for a medical illness, a trauma or fracture, and certain medications.
For women who have had a previous pregnancy-related DVT or those who have had a DVT associated with the hormone estrogen, taking an anticoagulant medication during pregnancy can help prevent future blood clots. To reduce the risk of a DVT most effectively, the typical recommendation is to take an anticoagulant during all subsequent pregnancies and for six weeks after a baby is born. The amount and the specific type of anticoagulant medication you need depend on a number of factors, including your weight, medical history and overall risk for developing another DVT.
Although taking an anticoagulant can lower your risk of another DVT significantly, it can’t eliminate the risk completely. To keep your risk as low as possible, take your anticoagulation medication exactly as prescribed. Lactation is permissible with most anticoagulants.
In general, regular exercise can help lower your risk of blood clots by enhancing blood flow and circulation throughout your body. Sitting for long periods of time limits blood flow and makes it more likely that a blood clot may form in one of your veins. For that reason, staying active during pregnancy is important, especially for patients with a history of DVT. Anecdotal recommendations include getting up and moving every one to two hours to promote blood circulation.
If you would like to keep running, discuss it with your obstetrician. He or she can help you decide on an appropriate level of activity for your situation. Even if running isn’t the best choice, it’s very likely you can participate in other activities that won’t increase your DVT risk and will help you stay fit and healthy throughout your pregnancy. — Dr. Carl Rose, OB-GYN, Mayo Clinic, Rochester, Minnesota
Related Articles