-
Mayo Clinic Q and A: Prostatitis — What is it and what can you do about it?
DEAR MAYO CLINIC: What causes prostatitis, and how is it diagnosed? Is it treatable?
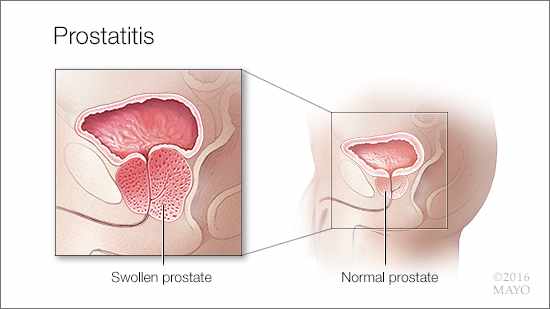
ANSWER: Prostatitis — a general term that encompasses a group of conditions characterized by swelling or inflammation of the prostate gland — generally isn’t life threatening. Although it’s less well-known than other prostate health concerns, such as prostate enlargement or prostate cancer, about 2 million American men visit their doctors for it each year. Some forms of prostatitis can be challenging to diagnose and treat.
The prostate is a walnut-sized gland located directly below the bladder in men. One of its main jobs is to produce fluid (semen) that nourishes and transports sperm. Irritation or inflammation of the prostate gland can occur for a number of reasons. Sometimes, bacteria-laden urine leaks from the urethra into the prostate, causing an infection. Use of a catheter or other instrument also can introduce infectious agents. In many cases of prostatitis, however, no clear cause can be found. It’s possible, though not proven, that other factors, such as trauma, increased pressure on the prostate, an overactive immune system or even excessive stress, can contribute to prostate irritation.
Prostatitis can cause a variety of symptoms, including a frequent and urgent need to urinate and painful or burning sensations while urinating. This often is accompanied by pelvic, groin or low back pain. If you experience any of these symptoms, see your doctor promptly to avoid complications, such as spread of the infection.
There are four types of prostatitis — two of which are caused by bacteria. Acute bacterial prostatitis usually comes on suddenly and can cause fever and chills in addition to pain and urinary symptoms. Chronic bacterial prostatitis also is caused by bacteria, but signs and symptoms typically develop more slowly and are less severe. Sometimes, it occurs as a complication of acute bacterial prostatitis that hasn’t been adequately treated.
Chronic pelvic pain syndrome (chronic prostatitis) symptoms are a lot like chronic bacterial prostatitis, but without the fever. In addition, tests show no sign of bacteria in the urine or in fluid from the prostate gland. In some cases, white blood cells found in a urine sample may signal the presence of inflammation. Although this is the most common form of prostatitis, it’s also the most challenging to diagnose and treat, because the cause is so uncertain.
Finally, asymptomatic inflammatory prostatitis doesn’t cause any symptoms and usually is found during an examination done for another reason. For example, prostatitis may increase the level of prostate-specific antigen (PSA) in your blood, which may be detected during a PSA screening test for prostate cancer. Asymptomatic prostatitis often doesn’t require treatment. But, if you need a repeat PSA test, your doctor may recommend a course of antibiotics first to clear the prostatitis.
To diagnose prostatitis, a urine sample may be collected to check for an infection. Unless the cause is clearly bacterial, prostatitis generally is diagnosed by feeling the prostate gland. To do this, your doctor inserts a gloved finger into your rectum and feels the outside wall of the gland. An inflamed prostate usually feels enlarged and tender. In some cases, a second urine sample may be collected after massaging the prostate, which forces fluid into the urethra. This fluid then can be examined for bacteria.
If neither bacteria nor white blood cells are found, your doctor may recommend further testing to rule out other conditions that may be causing your symptoms.
Prostatitis caused by bacteria can be treated with antibiotics. The length of treatment varies, depending on the type of prostatitis. While acute bacterial prostatitis usually can be treated with a four- to six-week course of antibiotics, chronic bacterial prostatitis is often more resistant to antibiotics and can take six to 12 weeks before the infection is cured. In some cases, a daily low-dose antibiotic may be needed indefinitely.
If you’re having difficulty urinating, your doctor may prescribe an alpha blocker to help relax the muscles connected to the bladder and prostate. Nonprescription pain relievers can help relieve pain and discomfort. Other therapies might include sitting and soaking in a warm bath (sitz bath), biofeedback (which can teach you how to control your bodily responses to certain stimuli), and physical therapy exercises. Acupuncture also may help prostatitis symptoms. (adapted from Mayo Clinic Health Letter) — Erik Castle, M.D., Urology, Mayo Clinic, Scottsdale, Arizona







