DEAR MAYO CLINIC: I have quite a few patches of skin that are much drier than others, including on my lower legs, knees and elbows. These areas get red and scaly sometimes, and itch on and off. Could this be psoriasis, or is it just extremely dry skin? At what point should I see my doctor about it?
ANSWER: From your description, it sounds like you could have psoriasis. Make an appointment to have your condition evaluated by a dermatologist — a physician who specializes in skin disorders. If it is psoriasis, your doctor can recommend treatment and give you advice on how to take care of your skin.
Psoriasis is a common skin condition that changes the life cycle of skin cells. It causes cells to build up rapidly on the surface of your skin. The extra skin cells can form thick, silvery scales and itchy, dry, red patches that can be painful. Psoriasis often goes through cycles, with symptoms flaring for a few weeks or months, and then going away for a time.
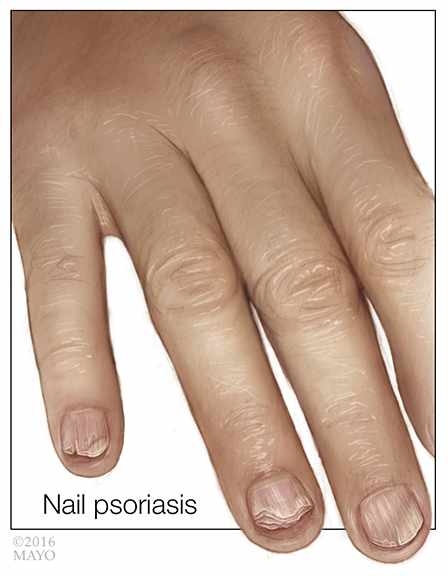
A dermatologist usually can diagnose psoriasis by reviewing your medical history and examining your skin, scalp and nails. Although it’s typically not necessary, your doctor also may recommend a biopsy. For this procedure, a small sample of your skin is removed and examined under a microscope to rule out other skin disorders. Conditions that can look like psoriasis include seborrheic dermatitis, lichen planus, pityriasis rosea and ringworm of the body.
If you have psoriasis, your dermatologist will talk with you about your treatment options. Psoriasis is a chronic condition, and, currently, there’s no cure. But, treatment can reduce symptoms by stopping the skin cells from growing so quickly. Therapies also can be used to remove scaly patches and smooth your skin.
If your condition is mild, you may only need to put a cream or ointment — sometimes called topical medication — on your skin to relieve your symptoms. Topical corticosteroids are a common psoriasis treatment. These anti-inflammatory drugs slow cell turnover by suppressing the immune system. That eases inflammation and relieves itching. Other topical medications also can be useful in treating psoriasis, including retinoids, anthralin, salicylic acid, synthetic forms of vitamin D, and coal tar, among others. Regardless of what medication you use, keeping your skin well-moisturized at all times will help control the dryness and discomfort of psoriasis.
When topical treatments alone aren’t enough to keep your symptoms in check, your dermatologist may suggest you also use light treatment, or phototherapy, to control psoriasis. The easiest form of phototherapy involves exposing your skin to controlled amounts of natural sunlight. Other forms of light therapy include the use of artificial ultraviolet A (UVA) or ultraviolet B (UVB) light. Although this treatment may be time consuming, it can be very effective.
If you have severe psoriasis or if it doesn’t respond to other kinds of treatment, your doctor may recommend oral or injected drugs, along with other therapies. In general, these drugs help lower the production of skin cells or reduce inflammation. They also may suppress your immune system.
Psoriasis sometimes can be challenging to manage. It may be unpredictable, going through cycles of improving and worsening symptoms without warning. In addition, treatment is not uniformly effective. What works well for some people might not work for others. Your skin may become resistant to some treatments over time, and the most potent psoriasis treatments can have serious side effects.
If your symptoms are due to psoriasis, you and your dermatologist can work together to develop a treatment plan. As you move forward with treatment, stay in contact with your doctor, especially if your condition doesn’t improve after starting treatment or if you’re having uncomfortable side effects. He or she can help you adjust your treatment to ensure the best possible symptom control. — Dr. Rokea el-Azhary, Dermatology, Mayo Clinic, Rochester, Minnesota