-
Mayo Clinic Q and A: Rare, inherited risk factor can result in emphysema and liver damage
 DEAR MAYO CLINIC: A family friend was recently diagnosed with emphysema, but he never smoked and was told that his condition was caused by alpha-1. What is this, and how is it diagnosed?
DEAR MAYO CLINIC: A family friend was recently diagnosed with emphysema, but he never smoked and was told that his condition was caused by alpha-1. What is this, and how is it diagnosed?
ANSWER: Emphysema is one of a group of lung diseases, including chronic bronchitis, that make up chronic obstructive pulmonary disease, or COPD. Tobacco smoking tops the list of emphysema risk factors. Less common risk factors include long-term exposure to dust or fumes. But there also are rare inherited risk factors, including alpha-1.
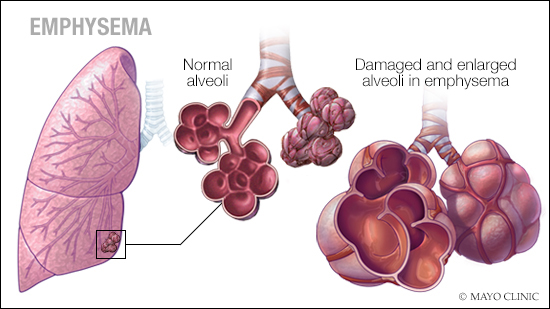
Emphysema involves long-term, permanent damage to the tiny clusters of air sacs (alveoli) in the lungs, where oxygen is absorbed into the bloodstream and carbon dioxide is released to be exhaled. Alveoli tissues are normally elastic, but emphysema results from destruction of the elastic tissue. This makes it harder to move air and ultimately results in shortness of breath that gets progressively worse over time.
Alpha-1 (also called alpha-1 antitrypsin deficiency or AAT deficiency) is diagnosed with a simple blood test. Normally, large amounts of the alpha-1 antitrypsin protein are made in the liver, released into the bloodstream and distributed to the body. This protein helps protect the lungs from damage and preserves the elasticity of lung tissues.
In those who have alpha-1 antitrypsin deficiency, an abnormal protein is made and it isn’t fully released by the liver into the bloodstream. Thus, the lungs lose a major protective element and become susceptible to emphysema even in people who never smoked and had only limited exposure to other lung irritants. For those who do smoke and have alpha-1 antitrypsin deficiency, smoking can greatly accelerate the damage that leads to emphysema. Moreover, buildup of the abnormal alpha-1 antitrypsin protein in the liver also can lead to permanent liver damage (cirrhosis) and is associated with liver cancer.
Breathing tests or chest imaging may be used to determine the severity of emphysema due to alpha-1 antitrypsin deficiency. Not everyone with the deficiency gets emphysema, so breathing tests and imaging can be important.
Alpha-1 protease inhibitors are a recent development in the treatment of alpha-1 antitrypsin deficiency. These inhibitors are infused blood products taken from healthy individuals that increase alpha-1 antitrypsin levels in the bloodstream. The therapy may slow lung damage, but can’t reverse damage. It’s very expensive and commonly involves weekly infusions and is typically available only to those who meet certain criteria.
A free, confidential testing program is available for family members of someone with alpha-1 antitrypsin deficiency. Details can be found on the Alpha-1 Foundation website. (adapted from Mayo Clinic Health Letter) — Dr. Michael J. Krowka, Pulmonary & Critical Care Medicine
****************************
Related Articles
- Mayo Clinic Q and A: Self-care steps and treatment can relieve COPD symptoms published 12/11/18
- Mayo Clinic Minute: What you need to know about COPD published 11/15/18
- New COPD guidelines from international panel provide updated recommendations published 9/19/18
- Science Saturday: Using biological particles from milk to target liver cancer published 7/14/18
- Mayo Clinic Q and A: Treatment for liver cancer published 3/20/18
- Sharing Mayo Clinic: Innovative radiation treatment slows liver cancer published 6/18/17







