-
Cancer
Mayo Clinic Q and A: Screening exams, breast self-awareness can be key to catching breast cancer early
DEAR MAYO CLINIC: Every year when I get my mammogram, the results are that the breasts are too dense to see small cancers. Why should I keep getting mammograms? Should I instead ask for an ultrasound to look for cancer? Also, are self-exams still recommended? You don’t hear much about them anymore.
ANSWER: Increased breast density can make interpreting mammograms difficult. Even if your breasts are dense, however, Mayo Clinic recommends an annual mammogram starting at age 40. Some women who are at a high risk for breast cancer may need to start screening earlier. Depending on your situation, your doctor may recommend additional screening tests, too. Breast self-exams are no longer formally recommended, but it is important for you to be familiar with your breasts’ typical appearance.
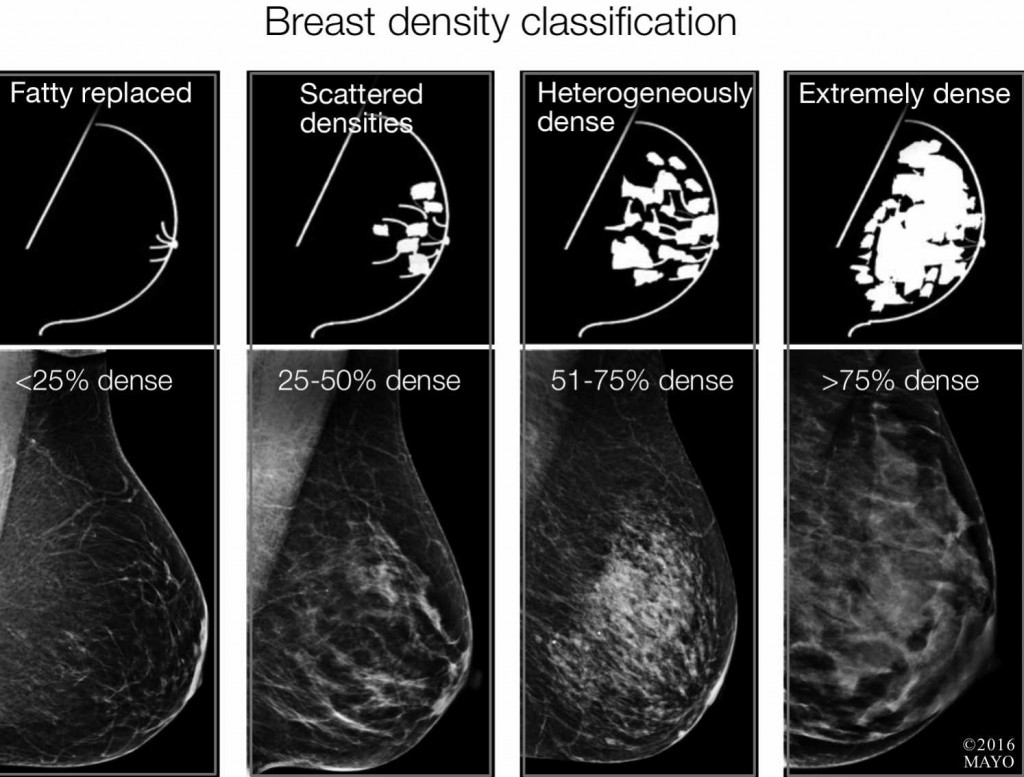
Breast tissue that is not dense contains fat and appears dark on a mammogram. Dense breast tissue is composed of milk glands, milk ducts and supportive breast tissue. Dense tissue appears white on a mammogram. There are four levels of breast density: fatty, scattered fibroglandular, heterogeneously dense and extremely dense. If you have heterogeneously or extremely dense breasts your breasts are considered “dense.” Some states require the level of breast density to be documented on your mammogram report.
Because both dense tissue and cancer appear white on mammogram images, a high level of breast density can obscure cancer on a mammogram. Mammograms, however, are still very useful for detecting breast changes that could indicate cancer, even in women who have dense breast tissue. Mammograms remain one of the most important tools in the fight against breast cancer. Studies of women in their 40s and 50s have shown that screening mammograms decrease breast cancer deaths by 15 to 20 percent.
Along with your annual mammogram, talk with your doctor about your individual breast cancer risk. Women with dense breasts may benefit from supplemental imaging, such as 3D digital breast tomosynthesis or molecular breast imaging. Women with a high risk for breast cancer may benefit from breast MRI.
Be mindful that there is a downside to some supplemental screening tests. The test could find an abnormality that requires further investigation which ultimately turns out benign, therefore subjecting you to the risk of an unnecessary medical procedure. Also, your insurance may not cover the cost of some supplemental screening studies, leaving you with an out-of-pocket expense. And finally, at this time research remains inconclusive about whether supplemental breast imaging reduces the rate of breast cancer deaths overall.
Some health care facilities do use handheld ultrasound testing to scan the whole breast. However, consistent, high-quality handheld ultrasound examinations of the entire breast are difficult to perform. Mayo Clinic does not use ultrasound as a supplemental screening tool to scan the entire breast for cancer. Mayo Clinic does use diagnostic ultrasound to investigate specific areas of the breast that look or feel abnormal or appear abnormal on a mammogram image.
In addition to screening exams, breast self-awareness can be key to catching breast cancer early. The breast self-exams that used to be routinely recommended are no longer used as part of breast cancer screening. That’s because research hasn’t shown a clear benefit. Still, you should be aware of the general appearance and feel of your breasts.
If you notice any of the following changes, report them to your doctor right away: a breast lump; a change in the texture of your breast tissue; breast skin changes, such as dimpling or redness; a change in the position of a nipple; change in breast symmetry; or discharge from a nipple.
For the best breast care, talk with your doctor about your cancer screening options. Together, you and your doctor can decide based on your individual risk factors what specific breast cancer screening tests are right for you. — Dawn Mussallem, D.O., Diagnostic Breast Specialist at The Robert and Monica Jacoby Center for Breast Health, Hematology/Oncology, Mayo Clinic, Jacksonville, Fla.