-
Health & Wellness
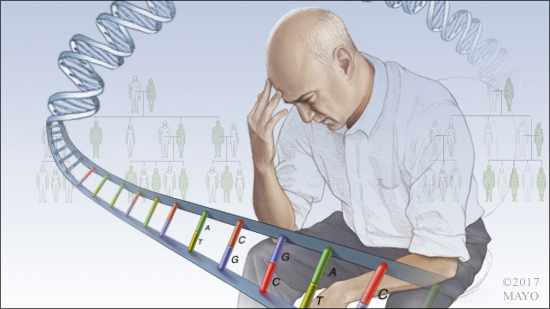
Mayo Clinic Q and A: Suicide and genetics — a complicated association
 DEAR MAYO CLINIC: Why does it seem that suicide tends to run in families? Does it have anything to do with genetics?
DEAR MAYO CLINIC: Why does it seem that suicide tends to run in families? Does it have anything to do with genetics?
ANSWER: The association between genetics and suicide is complicated. Research has shown that there is a genetic component to suicide. But it is only one of many factors that may raise an individual’s risk. And even if someone is at high risk for suicide, that doesn’t predict whether or not an individual will actually act on suicidal thoughts.
Genetic research, including studies involving twins, has revealed that many psychiatric conditions, including having suicidal tendencies, are influenced by genetics. While studies demonstrate that specific genes, such as one called the BDNF Met allele, can increase risk for suicide, it’s more likely that a range of genes affect connections and pathways within the brain, and impact suicide risk.
Complicating matters further, a process called epigenetics also comes into play when considering the effect of genes on suicide. This process controls when certain genes are turned on or off as a person grows and develops, and it can be influenced by what happens in a person’s environment.
For example, if someone goes through a difficult event as a child, that experience could have an impact on how or when a gene is activated within that person’s brain. Researchers speculate that negative experiences influencing epigenetics in a person who has a family history of suicide could further compound that person’s suicide risk.
In addition, it is known that 90 percent of people who die by suicide have a psychiatric illness at the time of death. Mood disorders, psychotic disorders, certain personality disorders and substance use disorders can increase suicide risk substantially. Each of those disorders has a genetic component, too.
It’s important to understand, however, that an increased risk of suicide does not predict who will commit suicide. For some people — even those whose genetics may seem to predispose them to a higher suicide risk — the thought of suicide doesn’t enter their minds. For others, suicide quickly may become a focus of their thoughts.
For those whose thoughts do turn to suicide, the way they arrive at suicidal thoughts may be a well-imprinted and familiar pathway. Psychotherapeutic treatment can help examine the process they go through to get to that point and find ways to interrupt the process.
Genetics, family history and environment all matter when it comes to the risk of suicide. But knowing risk factors is not a substitute for a thorough assessment of an individual’s situation and the process he or she takes to arrive at suicidal thoughts.
If you or a loved one are concerned about your risk for suicide, or if you’ve had suicidal thoughts, talk to a mental health professional. To help you find ways to break the cycle that leads to suicidal thoughts, he or she can work with you to treat any psychiatric illness that may be present and help you understand the process you’re going through when you turn to the possibility of suicide.
If you are in a suicide crisis or emotional distress, the Suicide & Crisis Lifeline provides free, confidential emotional support 24/7 by dialing 988. — Dr. Brian Palmer, Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota
Related Articles







