-
Featured News
Mayo Clinic Q and A: Surgical techniques used to treat rectal prolapse
 DEAR MAYO CLINIC: What is involved in the surgery to treat rectal prolapse, which is causing fecal incontinence? How long is the recovery?
DEAR MAYO CLINIC: What is involved in the surgery to treat rectal prolapse, which is causing fecal incontinence? How long is the recovery?
ANSWER: There are several techniques that can be used to perform surgery to treat rectal prolapse. The one that’s right for you depends on factors such as your medical condition and age, as well as your surgeon’s experience and expertise. After the surgery, most people return to their usual activities in about four to six weeks.
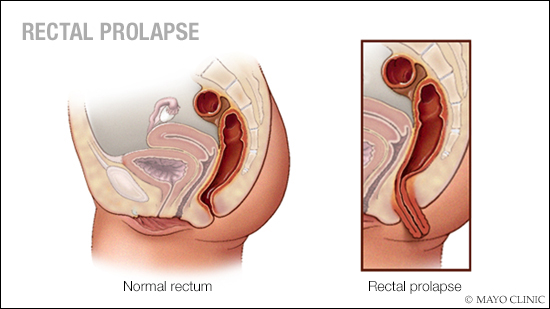
Rectal prolapse happens when the last part of the large intestine, called the rectum, stretches and comes out of the anus. This condition, which often is a result of chronic straining with bowel movements, can lead to fecal incontinence — a loss of bowel control and inability to hold in stool.
Surgery puts the rectum back in place and corrects rectal prolapse. Fecal incontinence may be improved after the surgery, but the procedure does not always eliminate that disorder. Additional treatment for fecal incontinence may be necessary after rectal prolapse surgery.
Rectal prolapse surgery can be done through the abdomen — a procedure called rectopexy — with a larger incision during open surgery or using laparoscopic methods that involve several smaller incisions. The surgery also can be performed via the region around the anus, called the perineum.
Surgery through the abdomen typically is used for younger patients who don’t have other medical issues. During this surgery, the surgeon places the rectum back in its proper position, and, using sutures or a mesh sling, the surgeon anchors the rectum to the back wall of the pelvis, called the sacrum. In some cases, a portion of the colon may be removed during surgery, and then the rectum is secured to the sacrum to keep it in place.
Rectal prolapse surgery performed through the perineum often is used for older patients who may not be able to undergo abdominal surgery due to other medical conditions. There are two ways to perform this procedure. During the more common approach, called the “Altemeier procedure,” the surgeon pulls the rectum through the anus; removes a portion of the rectum, along with the bottom part of the colon; and attaches the remaining rectum to the remaining colon.
Another method for repairing a rectal prolapse through the perineum, called the “Delorme procedure,” typically is done for short prolapses. The lining of the rectum is removed. Then the muscular layer is folded to shorten the rectum and eliminate the tissue that’s coming out of the anus.
Most patients spend a brief time in the hospital after surgery to recover and regain bowel function. The length of the hospital stay depends on which procedure is performed. Some people spend just one night in the hospital and go home the next day.
Drinking plenty of fluids, using stool softeners and eating a fiber-rich diet in the weeks after surgery can help avoid constipation and excessive straining that can lead to a recurrence of rectal prolapse. In some cases, physical therapy may be necessary to relearn how to use the pelvic floor muscles, which support the bladder and bowel. Most people are able to return to their usual activities within four to six weeks after rectal prolapse surgery.
If you’re considering rectal prolapse surgery, talk to your surgeon about the different surgical options. He or she can review the risks and benefits with you, and discuss what you can expect after surgery, including additional treatment for fecal incontinence, if needed. — Dr. Heidi Chua, Colon and Rectal Surgery, Mayo Clinic, Rochester, Minnesota







