-
Mayo Clinic Q and A: Thyroid cancer — treatment and prognosis
 DEAR MAYO CLINIC: How is thyroid cancer treated? Does it always require taking out the thyroid? When is iodine treatment used, and how does that work?
DEAR MAYO CLINIC: How is thyroid cancer treated? Does it always require taking out the thyroid? When is iodine treatment used, and how does that work?
ANSWER: Treatment for thyroid cancer usually involves removing all or part of the thyroid gland. In cases where thyroid cancer is advanced or aggressive, radioactive iodine treatment may be recommended after surgery to destroy any cancer cells that couldn’t be removed during surgery. For very small papillary thyroid cancers (less than 1 centimeter in diameter and completely confined to the thyroid on ultrasound examination), it may be reasonable to avoid surgery and monitor them periodically without treatment. This is termed “surveillance” and requires annual imaging of the thyroid with high-quality ultrasound. These small thyroid cancers are low risk for progression, especially in persons over 60.
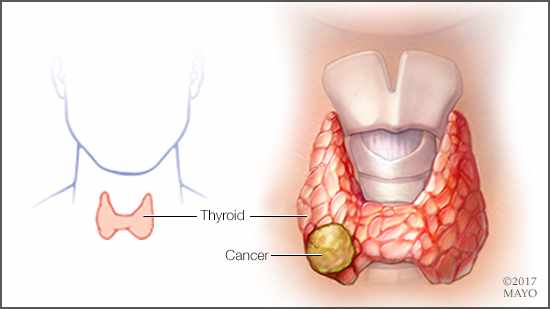
The thyroid is a butterfly-shaped gland located in the midline of your neck, about halfway between your Adam’s apple and your breastbone. Your thyroid gland produces two main hormones: thyroxine, or T4, and triiodothyronine, or T3.
Thyroid hormones impact many cells within your body. They maintain the rate at which your body uses fats and carbohydrates, help control your body temperature, affect the working of your nervous system, and influence your heart rate. Your thyroid gland also produces calcitonin, a hormone that helps regulate the amount of calcium in your blood.
Thyroid cancer is not common in the U.S. When it is found, though, most cases can be cured. Surgery to remove all or most of the thyroid — a procedure called a thyroidectomy — is often the first step in treatment.
Thyroidectomy typically involves making an incision in the center of the neck to access the thyroid gland directly. In addition to removing the thyroid, the surgeon may remove lymph nodes near the thyroid gland if the cancer is known or suspected to be spreading outside the thyroid. Then, those lymph nodes will be checked for cancer cells. An ultrasound exam of the neck before surgery can help doctors determine if lymph node removal is necessary.
When thyroid cancer is found in its earliest stage, and the cancer is very small, it may only be necessary to remove one side, or lobe, of the thyroid, and leave the rest in place. In that situation, the thyroid still can function and produce hormones.
When the entire thyroid is removed, lifelong thyroid hormone therapy is required to replace the thyroid's natural hormones and regulate the body's metabolism. In addition to supplying the missing hormone the thyroid normally makes, this medication also suppresses the pituitary gland’s production of thyroid-stimulating hormone, or TSH. That’s useful, because there’s a possibility that high TSH levels could foster the growth of any remaining cancer cells.
If thyroid cancer is found in its later stages, if it’s a more aggressive form of cancer, or if it is cancer that has come back after earlier treatment, then radioactive iodine therapy may be recommended after the thyroid has been removed.
Radioactive iodine comes in a capsule or liquid that’s swallowed. The therapy works because thyroid cells naturally absorb iodine. So when the medicine is taken up by any remaining thyroid cells or thyroid cancer, the radioactivity destroys those cells. Because the thyroid is the primary site where iodine is absorbed by the body, there’s a low risk of harming other cells with this treatment. Afterward, the radioactive iodine leaves the body through urine.
If thyroid cancer is not cured with a combination of surgery and radioactive iodine therapy, then chemotherapy, external radiation therapy or other treatment may be necessary. Fortunately, surgery cures most cases of thyroid cancer, and the long-term outlook after the procedure is usually excellent. — Dr. John Morris III, Endocrinology, Mayo Clinic, Rochester, Minnesota