-
Mayo Clinic Q and A: Treating colon cancer
DEAR MAYO CLINIC: A family member recently was diagnosed with colon cancer. After researching potential treatment options, I came across intraoperative radiation therapy. What is the difference between this and normal radiation? Is radiation a standard treatment option, or are there other approaches?
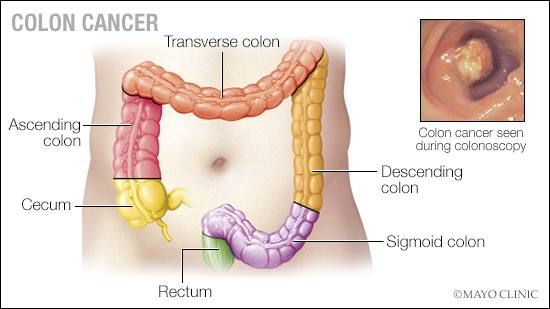
ANSWER: Colon cancer is one of the most common malignancies in the U.S., with more than 100,000 new cases diagnosed each year. Over a lifetime, it is estimated that 1 in 23 men and 1 in 26 women will be diagnosed with colon cancer. Typical colon cancers start as a polyp-like growth in the inside layer of the colon, which can be seen during a colonoscopy. Most cancer organizations recommend starting colonoscopy screenings at age 45.
When a mass is found during a colonoscopy or cancer is suspected, biopsies are taken and reviewed by a pathologist. In this scenario, most patients are asymptomatic. Without preventive colon cancer screenings, a tumor may grow to an advanced stage before it causes any symptoms that a patient or health care professional would recognize. The most common signs and symptoms of colon cancer are anemia, which may lead to fatigue; abdominal pain; blood in the stool or other bowel changes; weight loss; and signs of obstruction.
Once colon cancer is diagnosed, the next step is a staging examination. This involves a history and physical examination; blood work; confirmation that a full colonoscopy has been performed; and CT scans of the chest, abdomen and pelvis. The results of these tests will allow your health care professional to assign a clinical stage. In stages 1 and 2, the tumor remains in the colon wall with no evidence that it has spread further. With stage 3, there is concern that the tumor cells have spread to the regional lymph nodes, and in stage 4 colon cancer, the tumor cells have spread outside of the local area to other organs — most commonly the liver, lungs or peritoneum.
Surgery is the mainstay of treatment for stages 1, 2 and 3 disease and is usually the first step in the treatment process. The segment of the colon bearing the tumor is removed, along with the draining lymph nodes. The ends of the intestine are reconnected, and the specimen is sent to the pathologist who then performs a histologic examination of the colon and the associated lymph nodes. The pathologist will assign a final pathologic stage to the tumor, which will dictate the need for any additional treatment.
For stage 1 colon cancer, the treatment is complete after surgery — no additional treatment is necessary. Patients are closely followed with physical examinations and blood tests for several years. Patients diagnosed with stage 2 disease should meet with a medical oncologist to determine whether chemotherapy is necessary after recovering from surgery. Patients with pathologic stage 3 colon cancer will be advised to receive chemotherapy after surgical recovery and should meet with an oncologist in the early postoperative setting. For all colon cancer patients, it is essential to continue regular colonoscopies to rule out any recurrence at the site of the prior colon resection, and to find and remove small polyps that may form in the future.
Stage 4 disease is more complicated. Treatment is individualized for each patient with a team that includes medical oncologists and, sometimes, surgeons.
It is uncommon to use radiation therapy for the management of colon cancer. However, it may be recommended for patients with locally advanced disease where the cancer is growing into multiple organs in the abdomen or for patients with extensive lymph node involvement along the aorta. Typically, when radiation is needed, external beam radiation is given in multiple doses before surgery is performed. The standard course of treatment is 28 short sessions where the radiation targets the tumor-bearing region. Then, a patient will have a waiting period of approximately six weeks before surgical removal of the tumor.
When the treatment team is concerned about achieving negative margins, or removing the entire tumor with an edge of normal tissue around the specimen, intraoperative radiation therapy may be considered. Intraoperative radiation therapy rarely is used for colon cancer, but, when necessary, the area of concern is directly targeted with a single fraction of radiation during surgery. This allows more precision to the affected area with limited damage to the surrounding tissue. Intraoperative radiation therapy is not used in isolation. It is planned and used in combination with the external beam radiation that is administered preoperatively.
It is important to seek surgical treatment from highly experienced surgeons at a center, like Mayo Clinic, that does many of these operations. Although a diagnosis of advanced colon cancer can be frightening, turning to a surgical oncologist experienced with colon cancer can help ensure that all available treatment options are being considered to provide the best outcome for your loved one. — Dr. Kellie Mathis, Colon and Rectal Surgery, Mayo Clinic, Rochester, Minnesota
****************************
Related Articles
- Mayo Clinic Minute: Why millennials should know colon cancer symptoms published 3/3/23
- Mayo Clinic Q and A: Advances in screening for colon cancer published 12/29/22
- Science Saturday: Mayo Clinic patient grateful after genetic test leads to unexpected, early detection of colon cancer published 9/3/22
- Mayo Clinic Q and A: Polyps are possible culprits in colon cancer published 4/21/22
- Consumer Health: Colon polyps and colon cancer screening published 3/18/22