-
Featured News
Mayo Clinic Q and A: Treating inflammatory bowel disease
 DEAR MAYO CLINIC: A year after colon resection for inflammatory bowel disease, I am still having two or three uncontrollable loose movements a day. I take an anti-diarrhea medication, but it does not seem to help. Should I be concerned, and what are my options at this point?
DEAR MAYO CLINIC: A year after colon resection for inflammatory bowel disease, I am still having two or three uncontrollable loose movements a day. I take an anti-diarrhea medication, but it does not seem to help. Should I be concerned, and what are my options at this point?
ANSWER: Your condition needs to be reassessed at this time. Make an appointment to see your gastroenterologist to discuss and evaluate your symptoms. You may need additional imaging exams or other testing to help develop an appropriate treatment plan for your situation.
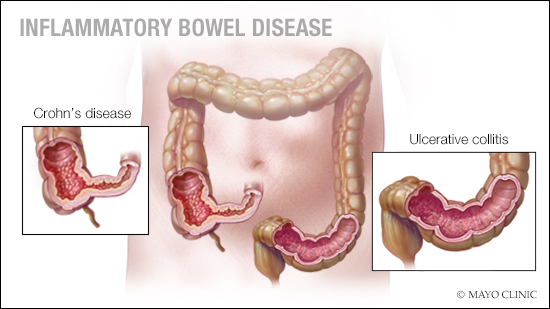
Inflammatory bowel disease, or IBD, is a term used to describe chronic inflammation of the digestive tract. There are several types of inflammatory bowel disease, including ulcerative colitis and Crohn's disease. These disorders often cause severe diarrhea, along with other symptoms, such as weight loss, abdominal pain and fatigue.
When more conservative treatment, such as medication, diet modification and lifestyle changes, aren't enough to control inflammatory bowel disease symptoms, surgery to remove part or sometimes all of the colon, called "colon resection," may be necessary.
It is not possible to tell from your question what kind of inflammatory bowel disease you have (ulcerative colitis or Crohn’s disease). As the types of surgery are different for each, it is only possible to make general statements. In some cases, colon resection is all that's needed to control inflammatory bowel disease symptoms. But when symptoms such as chronic diarrhea persist despite surgery, as in your case, it's important to seek follow-up care.
Talk to your gastroenterologist about the symptoms you're experiencing. Depending on the specifics of your surgery, it's possible that diarrhea could be a normal postoperative issue. For example, diarrhea sometimes can be the result of surgery when a considerable amount of the colon is taken out. It's also possible, however, that your disease has come back, and you need additional treatment.
Along with a review of your symptoms and a physical exam, you'll need some form of flexible endoscopy (e.g., colonoscopy or pouchoscopy), depending on how much colon was removed. Or you may need an imaging exam, such as an X-ray or CT scan, so your health care provider can evaluate your digestive tract to check for signs of disease recurrence.
If the tests show that your disease has come back, you'll need to be treated. The details of your treatment plan will depend on your situation, but it likely will involve drug therapy or additional surgery. The objective will be to not only relieve your symptoms, but also reduce your risk of further complications and achieve long-term remission of the inflammatory bowel disease.
If your disease hasn't come back, you and your gastroenterologist can discuss ways to better manage chronic diarrhea. You might need to change the dose and type of anti-diarrhea medication you're taking. Diet and lifestyle modifications also can reduce your symptoms. Talk to your health care provider or ask for a referral to a dietitian to learn about how you may be able to change your diet to ease diarrhea.
Keep in mind, too, that ongoing follow-up care is key to managing your condition successfully. Make sure you know the type of follow-up you need. Ask your gastroenterologist how often you should have checkups, as well as colonoscopies or other tests. Find out whom to contact with questions in between your appointments, and understand the symptoms or situations that should prompt you to seek medical care.
It's not always possible to cure inflammatory bowel disease, but long-term remission is achievable for many people with inflammatory bowel disease. Working closely with your care team to monitor your condition regularly and promptly address issues related to your disease will make it more likely for you to be able to reach that goal. — Dr. Tonia Young-Fadok, Colon and Rectal Surgery, Mayo Clinic, Scottsdale, Arizona
****************************
Related Articles
- Crohn’s disease is an inflammatory bowel disease published 9/27/18
- Mayo Clinic Q and A: Could this be the cause of your persistent diarrhea? published 6/26/18







