-
Featured News
Mayo Clinic Q and A: Treating melasma
DEAR MAYO CLINIC: Years ago, I had some patches of melasma on my face removed with IPL treatment. When I went to make an appointment with my dermatologist recently for the same condition, I was told IPL should not be used for melasma. Why is this? What treatment should be used?
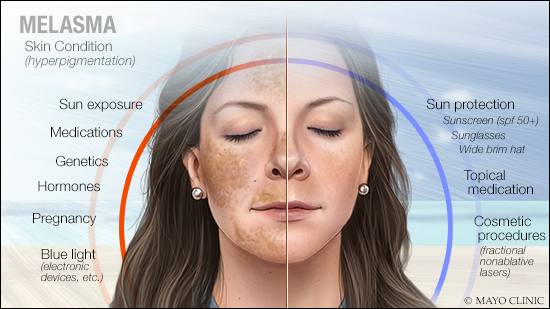
ANSWER: The skin condition melasma can be challenging to get rid of completely, and as a chronic condition, it can come back after treatment. With the treatment you mention, intense-pulsed light or IPL, melasma often reappears quickly. Intense-pulsed light also carries a risk of heating the surrounding skin, which is thought to worsen melasma. To treat melasma, sun protection, topical medications and cosmetic procedures often are combined to achieve the best results.
Melasma is a common condition that appears as irregular patches of tan, brown or brown-gray pigmentation, usually on the face. Melasma affects women much more frequently than men. Patients with darker skin also are more likely to develop melasma.
The most common trigger for melasma is ultraviolet light from sun exposure. Melasma may develop as a result of hormone changes due to pregnancy or certain medications, such as oral contraceptives. Recently, research has found that blue light emitted from light bulbs, computer screens and other electronic devices can worsen melasma. Melasma tends to run in families, which points to a genetic component of this disorder, too.
When facial pigmentation first appears, it’s important to see a dermatologist for a definitive diagnosis because melasma may be subtle and can look like other skin conditions. Once diagnosed, the goal of melasma treatment is to decrease the production of pigment and remove areas of excess pigmentation that already have appeared.
Intense-pulsed light treatment for melasma uses a broad spectrum of light to generate heat to target and remove pigment. But the heat diffuses to all the surrounding tissues. That can lead to complications, including a condition known as post-inflammatory hyperpigmentation, which causes more dark patches to appear. Research shows that intense-pulsed light can improve melasma in the short term, but relapse often is seen within three months.
More recently, fractional nonablative lasers have been studied for the treatment of melasma. These lasers resurface the skin and remove pigment through heated columns, but they leave the skin around the columns untouched. Different devices with different levels of power are available, so the treatment can be individualized for each patient. Unlike the set 100% coverage of intense-pulsed light, these lasers can treat as low as 5% of the skin to slowly remove pigment with a much lower risk of relapse or worsening of melasma.
When considering melasma treatment overall, however, topical treatment is the key to success. It should be used before any light or laser procedure and, to decrease the risk of relapse, it should be continued even when those procedures are recommended. Topical hydroquinone is the most common lightening agent used. It works by decreasing the production of pigment. Your doctor may recommend combining it with tretinoin, corticosteroids, antioxidants or other topical products for added efficacy. In some cases, superficial chemical peels also may be considered to remove pigment.
Avoiding sun exposure and protecting your skin from the sun is absolutely essential to prevent further development of melasma and to maintain treatment results. That includes wearing a wide-brimmed hat and sunglasses when you’re outdoors, and using sunscreen with a sun protection factor (SPF) of 50 or higher on a daily basis. A sunscreen with a physical blocker, such as zinc oxide or titanium dioxide, is best. Reapply it every one to two hours.
Research into melasma treatment is moving forward. Recent data has identified that melasma is associated with inflammation, skin barrier breakdown and an increase in blood vessels. Those findings may inform new treatment options. Talk to your dermatologist to learn more about topical and oral treatments on the horizon. — Dr. Elika Hoss, Dermatology, Mayo Clinic, Scottsdale, Arizona







