-
Cardiovascular
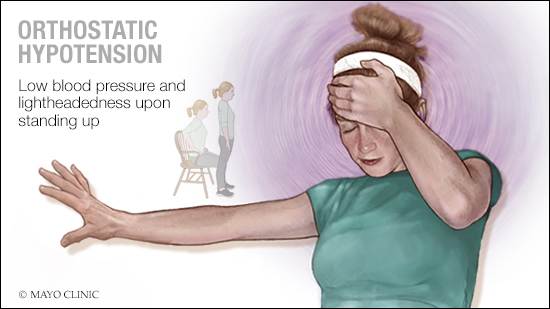
Mayo Clinic Q and A: Treating orthostatic hypotension
 DEAR MAYO CLINIC: Is it always possible for doctors to determine what causes orthostatic hypotension? How is it treated?
DEAR MAYO CLINIC: Is it always possible for doctors to determine what causes orthostatic hypotension? How is it treated?
ANSWER: The cause of orthostatic hypotension usually can be identified. That’s important because understanding the cause allows treatment to be tailored to an individual’s specific situation. The goals of treatment for orthostatic hypotension are to prevent blood pressure from falling too low and improve quality of life. Treatment targets the underlying cause and low blood pressure itself.
Orthostatic hypotension is a form of low blood pressure that happens when you stand up from sitting or lying down. When you stand up, blood tends to pool in your legs and belly. Your body compensates for that by increasing your heart rate and constricting blood vessels, so enough blood returns to the heart and is sent to your brain.
If you have orthostatic hypotension, that process doesn’t happen the way it should. Instead, when you stand up, your blood pressure drops, often leading to lightheadedness, dizziness, headaches, fatigue, blurred vision and sometimes fainting.
Orthostatic hypotension can develop for many reasons. It could be the result of something as simple as dehydration or as complex as a nervous system disorder. Diabetes is a common cause of orthostatic hypotension. Rarer causes include heart valve disorders, amyloidosis, extremely low heart rate, Addison’s disease and Lewy body dementia. Some medications may cause orthostatic hypotension.
Investigation into the cause of orthostatic hypotension begins with a review of your medical history, discussion of your symptoms and a physical exam. But the cause usually cannot be identified based on those factors alone. Additional testing is needed to gather more information.
One simple test that must be done first involves measuring blood pressure standing up and comparing that to blood pressure lying down. Orthostatic hypotension is defined as a sustained drop in blood pressure by at least 20 millimeters of mercury in systolic blood pressure (the top number in a blood pressure reading) within three minutes of standing up.
In about one-third of cases, orthostatic hypotension is related to a problem in the body’s autonomic nervous system. In those cases, the disorder is referred to as “neurogenic.” Three features of neurogenic orthostatic hypotension are a large drop in blood pressure upon standing, a smaller-than-expected increase in heart rate when standing up, and inadequate blood pressure recovery after a Valsalva maneuver — a test where you breathe out against resistance.
One test used to assess the autonomic nervous system in people with orthostatic hypotension is a tilt table test. It evaluates how your body reacts to changes in position. During that test, you lie on a table that tilts to raise the upper part of your body, and your blood pressure is taken frequently as the table moves. Another test involves using an inflated cuff wrapped around one finger to measures blood pressure with each heartbeat. It allows a neurologist to assess how the autonomic nervous system is responding moment by moment.
Depending on the underlying condition suspected of causing orthostatic hypotension, your health care provider may recommend other tests. For example, you may need blood tests or tests that assess heart function, such as an EKG, stress test or echocardiogram.
Based on the results of the evaluation, treatment is geared toward addressing the underlying cause. When orthostatic hypotension is caused by a medication, changing the dose or switching medications may be all that’s needed to relieve symptoms. Sometimes lifestyle changes, such as drinking more water, adding salt, limiting alcohol and standing up slowly, can ease orthostatic hypotension.
Treatment for orthostatic hypotension must be individualized because regulating blood pressure is complex. And many people have a combination of orthostatic hypotension and high blood pressure, which makes treatment a balancing act. But with a comprehensive evaluation, the cause of orthostatic hypotension can be identified, and using a careful clinical approach, the condition often can be effectively managed. — Dr. William Cheshire, Neurology, Mayo Clinic, Jacksonville, Florida
****************************
Related Articles
- Mayo Clinic Q and A: When does fainting require medical attention? published 4/13/18
- Mayo Clinic Q and A: Orthostatic hypotension is more than feeling dizzy every now and then published 7/8/17







