-
Mayo Clinic Q and A: Treatment for Hurthle cell thyroid cancer
 DEAR MAYO CLINIC: Is it common to only have a partial thyroidectomy to remove Hurthle cells? My doctor is recommending this procedure, but I wonder if I should have my entire thyroid removed instead to eliminate the risk of the cancer coming back. Would it be better to have a total thyroidectomy?
DEAR MAYO CLINIC: Is it common to only have a partial thyroidectomy to remove Hurthle cells? My doctor is recommending this procedure, but I wonder if I should have my entire thyroid removed instead to eliminate the risk of the cancer coming back. Would it be better to have a total thyroidectomy?
ANSWER: A partial thyroidectomy can be an appropriate treatment for Hurthle cell thyroid cancer in some cases. The decision to undertake partial versus total thyroid removal depends on several factors, including the size and location of the tumor, as well as your individual medical situation.
Hurthle cell thyroid cancer is an uncommon cancer that's also called oxyphilic cell carcinoma. The cause of Hurthle cell cancer isn't clear, but generally it affects women and older adults more often than others. It typically does not run in families. This type of cancer tends to be more aggressive than the most common type of thyroid cancer, papillary thyroid cancer. Because there is potential to cure Hurthle cell thyroid cancer with surgery alone in many cases, removing part or all of the thyroid gland is the most common treatment.
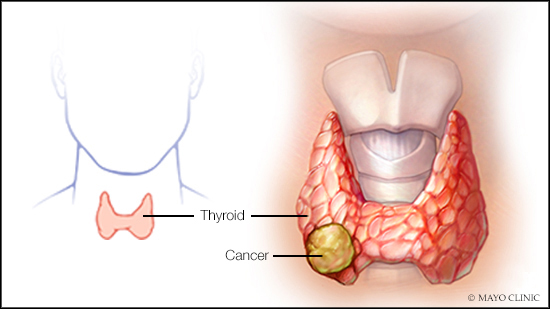
The thyroid gland is a butterfly-shaped gland located at the base of your neck, next to your windpipe. It makes hormones that regulate all aspects of your body's metabolism, from your heart rate to how quickly you burn calories.
A partial thyroidectomy involves removing only a portion of the gland — usually one lobe or one side of the thyroid. This procedure may be recommended when a Hurthle cell tumor is small (about 4 centimeters or less, and especially if a tumor is less than 2 centimeters), providing that the cancer is clearly located in one lobe of the thyroid and has not spread outside of the thyroid gland.
The potential benefit of a partial thyroidectomy over a total thyroidectomy is that the thyroid gland may be able to continue functioning normally after the procedure without taking thyroid hormone therapy to replace the hormones your thyroid usually produces.
For a total thyroidectomy, the surgeon removes all, or nearly all, of the thyroid gland tissue. Tiny remnants of thyroid tissue are left behind, however, near critical structures that need to be preserved, including nerves and the parathyroid glands. Surrounding lymph nodes might be removed if there's evidence that the cancer may have spread to them.
If your entire thyroid is removed, your body can't make thyroid hormone. If you don't take hormone replacement, you'll develop signs and symptoms of underactive thyroid, a condition called hypothyroidism. Thyroid hormone replacement is critical in the event of complete removal of the thyroid gland. The hormone replacement is equivalent to the hormone normally made by your thyroid gland and performs the same functions. Your doctor can determine the amount of thyroid hormone replacement you need based on blood tests.
Regardless of whether you have a partial or total thyroidectomy, there will be some risk of the cancer coming back, and you'll likely need follow-up appointments on a regular basis to check for cancer recurrence. Depending on your circumstances, however, the risk may be low. It's possible that there may be no difference in recurrence risk when comparing partial with total thyroid removal.
As you consider your options, it's best to seek care from an expert thyroid surgeon who sees a high volume of Hurthle cell cancer cases — ideally completing more than 20 or 30 thyroid surgeries a year. Complications from the surgery are generally lower when more experienced thyroid surgeons are involved. In addition, the expertise of the surgeon will help guide your decision to proceed with a partial versus total thyroidectomy. — Dr. Keith Bible, Medical Oncology, Mayo Clinic, Rochester, Minnesota







