-
Health & Wellness
Mayo Clinic Q and A: Treatments for vaginal atrophy can prevent complications
DEAR MAYO CLINIC: I have been in menopause for about a year and have not had many problems other than what my doctor diagnosed as vaginal atrophy. Do over-the-counter products usually help relieve the symptoms, or will I need hormone therapy?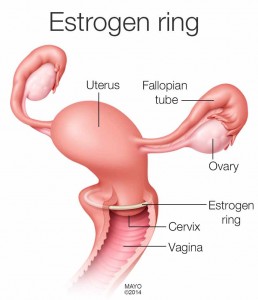
ANSWER: What you are experiencing is common. By some estimates, loss of lubrication and elasticity in the vaginal area (vaginal atrophy) affects at least half of women in midlife and beyond. Systemic hormone therapy — taken as an oral pill or a skin patch — isn’t the only treatment for menopausal vaginal atrophy. Other treatments are specific for vaginal atrophy. In fact, if you experience only vaginal symptoms related to menopause, without hot flashes and night sweats, these other therapies are probably better choices.
Vaginal atrophy is caused by a decrease in estrogen production. As you approach menopause, your body’s production of estrogen — the main female hormone — ebbs and flows and eventually decreases permanently. Less estrogen can make your vaginal tissues thinner, drier, less elastic and more fragile. Estrogen reduction and vaginal atrophy may also occur as the result of certain medical treatments, such as the removal of both ovaries, pelvic radiation, chemotherapy or hormonal treatment for breast cancer.
For some women, vaginal atrophy due to menopause may begin during the years leading up to menopause. For others, it may not become a problem until several years into menopause. Some women are never bothered by it.
Signs and symptoms of vaginal atrophy often include dryness, soreness, itching, burning, bleeding and pain during sex. Vaginal atrophy can also be a risk factor for an overactive bladder, stress incontinence and repeated bladder infections. And unlike hot flashes and night sweats — which tend to eventually go away on their own — vaginal atrophy can worsen without treatment. Left untreated, changes to vaginal tissue — such as a narrowed opening, loss of elasticity and easy bleeding — can become permanent. Worsening atrophy can lead to avoidance of sex, which can lead to further atrophy.
For mild symptoms, the first thing you might try is vaginal moisturizers and lubricants, which are available without a prescription. Vaginal moisturizers used every few days can help maintain the moisture of vaginal tissues. Lubricants can be used as needed for sexual activity. Vaginal lubricants can help decrease pain during sexual activity and can be applied as often as needed during sex. If you’re using condoms, avoid lubricants that aren’t listed as safe with condoms.
Regular sexual activity itself helps to maintain active blood flow to the vagina and helps produce vaginal lubrication. Stimulation with a lubricated vaginal dilator or vibrator also may help maintain vaginal health and prevent or reverse vaginal narrowing.
If nonhormonal therapies aren’t enough to relieve symptoms, your doctor may recommend a vaginal estrogen cream, tablet or ring. These use a much lower dose of estrogen than do systemic hormone therapies and thus limit your overall exposure to estrogen and its associated risks. Vaginal estrogen therapies help to reverse vaginal tissue changes by restoring the vagina’s normal pH balance, thickening surface tissue, increasing blood flow and lubrication. They can also help reduce urinary tract infections and overactive bladder symptoms. Vaginal estrogen therapies typically work better for moderate to severe symptoms than do nonhormonal therapies or even systemic hormone therapy.
An oral estrogen tablet is available for women who don’t want to use a vaginal product; however, it isn’t approved for those with or at high risk of breast cancer or who have had a uterine cancer.
Don’t put off seeking help for vaginal atrophy. There are treatments that can help you feel better and prevent complications. Talk to your doctor to determine if one of them may work for you. (adapted from Mayo Clinic Health Letter) — Mary Marnach, M.D., Gynecology, Mayo Clinic, Rochester, Minn.
Related Articles







