-
Featured News
Mayo Clinic Q and A: Understanding ischemic colitis
DEAR MAYO CLINIC: Is there a way to determine what causes ischemic colitis? Is it likely to return if someone has had it before?
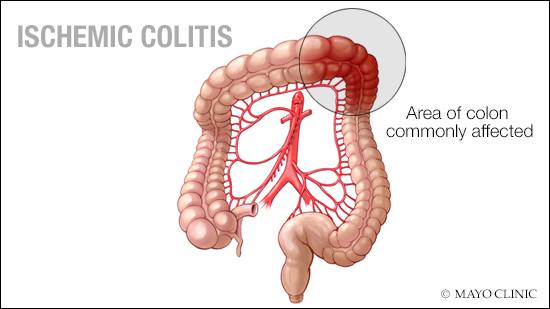
ANSWER: The cause of ischemic colitis, a condition in which blood flow to part of the large intestine (colon) is reduced, often is not clear. The condition occurs when there is a blocked or narrowed blood vessel (occlusive), or when there is a temporary decrease in blood flow to the colon (nonocclusive). Most cases of ischemic colitis are due to a nonocclusive mechanism. When this occurs, the colon temporarily receives less blood flow than usual, which then leads to areas of colon inflammation and ulceration. Fortunately, with proper medical care, most people diagnosed with ischemic colitis typically recover in a day or two, and never have another episode.
The colon receives less blood flow than any other portion of the gastrointestinal tract, even under normal conditions. So if the colon is suddenly subjected to reduced blood flow for whatever the reason, the tissue may be damaged. The severity of this damage depends on the amount of time that the blood flow was interrupted and the extent of the decrease. In rare cases, individuals can suffer a perforation, or tear, of the colon, which requires surgical treatment.
A number of situations can result in reduced blood flow to the colon. One cause is narrowing of arteries serving the colon, which often is associated with the buildup of fatty deposits (atherosclerosis). More commonly, decreased blood pressure due to dehydration, heart disease, severe illness, various medications, cocaine use or hemodialysis can decrease blood flow to the colon and cause an episode of ischemic colitis. Patients who participate in strenuous exercise can develop ischemia, likely due to a combination of dehydration and diversion of blood away from the colon to more vital parts of the body.
Abdominal surgeries that require clamping off arteries that supply the colon with blood, such as during repair of an aortic aneurysm, also may result in ischemic colitis. Blood clots in the vessels supplying the colon may be due to an underlying clotting disorder or could have traveled from another part of the body, such as the heart.
Although most people who develop ischemic colitis are over 55, younger patients can develop the condition. When ischemic colitis occurs in younger patients, a potential clotting disorder should be investigated.
The most common symptoms of ischemic colitis are abdominal pain, typically on the left side of the abdomen, and bloody diarrhea, which usually develops within 24 hours of the onset of pain. If a CT scan is performed, results can be normal or can show typical findings of bowel wall thickening of the affected portion of the colon. Bowel wall thickening is a nonspecific finding, however, that also could be the result of a bacterial infection of the colon; diverticulitis; or inflammatory bowel disease, an autoimmune condition.
Diagnosing ischemic colitis is best done through an evaluation with flexible sigmoidoscopy or colonoscopy. These tests can directly evaluate the lining of the colon and be used to obtain samples, or biopsies, of the colon tissue. Ischemic colitis tends to improve without treatment in 24–48 hours. In more severe cases, however, treatment may involve a day or two in the hospital for observation, IV fluids, and supportive care. Antibiotics also may be given in severe cases. Surgery only rarely is necessary if the colon has been damaged. For most people, the colon heals completely in about two weeks. But healing in a small percentage of people may take longer. — Dr. Sarah Umar, Gastroenterology, Mayo Clinic, Scottsdale, Arizona







