-
Gastroenterology
Mayo Clinic Q and A: What is inflammatory bowel disease?

DEAR MAYO CLINIC: I've had stomach issues my whole life, and it seems like my trips to the bathroom are becoming more frequent lately. I've heard of IBD. What is it? What are its symptoms? What can help me if I am diagnosed?
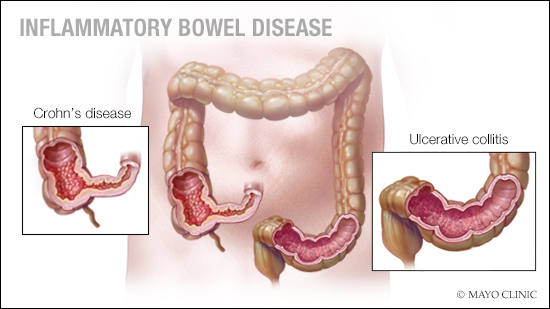
ANSWER: Inflammatory bowel disease (IBD) is a chronic inflammatory condition that usually impacts the gastrointestinal tract. IBD is an umbrella term for either ulcerative colitis or Crohn's disease, which are two different conditions with similar origins and inflammatory processes that affect the gastrointestinal tract. Ulcerative colitis involves inflammation along the superficial lining of the large intestine (colon) and rectum while Crohn's disease involves inflammation and ulcers that can involve the deeper layers of the digestive tract. This can affect anywhere from the mouth to the anus, but most commonly affects the last part of the small intestine and/or the colon.
Symptoms are variable and may sometimes be nonspecific, but the most common symptoms that patients experience are diarrhea, bloody stools and abdominal pain. Some patients might experience fatigue, fever, unintentional weight loss and joint pain. In some cases, patients develop extraintestinal (organs beyond the intestines) manifestations which can affect different organs in the body such as the eyes, skin, joints or liver.
Most people with IBD are diagnosed before their 30s, but some won't develop the disease until their 50s or older. To diagnose someone with IBD, a patient presents their symptoms to their primary care clinician or gastroenterologist, who takes a thorough history to try to better understand how long the symptoms have been going on. This would lead the healthcare professional to order further testing, which can include an endoscopic evaluation such as a colonoscopy. Biopsies taken during a colonoscopy are needed to confirm a diagnosis of inflammatory bowel disease.
Currently, there is no cure for inflammatory bowel disease. However, there are many treatment options, including medical, surgical and dietary interventions that can help. The goal of treatment is remission, which means eliminating all the inflammation and getting back to what looks like a normal colon or intestine. The treatment options we use differ from patient to patient depending on the severity and location of the disease. The decision on treatment is shared between the healthcare team and the patient.
Leaving inflammation untreated can lead to further complications. For example, if someone has persistent inflammation in their colon, that increases the risk for colon cancer. If someone has Crohn's disease, they're at increased risk of persistent inflammation causing something called strictures, which is narrowing in the colon or small intestine. Whenever there is a narrowing, it increases the risk of bowel obstruction, which would require surgery to help the bowels open up. This is why we are diligent in getting the right treatment to the patient and getting them to remission.
When it comes to IBD, diet is a question on everyone's mind. We do not have a specific diet for IBD, but we know that focusing on anti-inflammatory foods and antioxidants and avoiding processed foods, which can cause inflammation, is beneficial. One diet that I always recommend to most of my patients is the Mediterranean diet. The Mediterranean diet is a well-balanced diet that has a lot of anti-inflammatory products and antioxidants in it, so it could be very beneficial for patients who have IBD. Talk to your healthcare team about what is right for you. — Victor Chedid, M.D., Gastroenterology, Mayo Clinic, Rochester, Minnesota







