-
Featured News
Mayo Clinic Q and A: Why pancreatic cysts usually are not worrisome
 DEAR MAYO CLINIC: What could cause cysts on the pancreas? Can they become cancerous?
DEAR MAYO CLINIC: What could cause cysts on the pancreas? Can they become cancerous?
ANSWER: The reason cysts develop on the pancreas isn’t known. But they appear to be related to the aging process, because they become more common as people get older. Most pancreatic cysts are harmless cysts that never lead to health problems or require treatment. Only in rare instances do pancreatic cysts become cancerous.
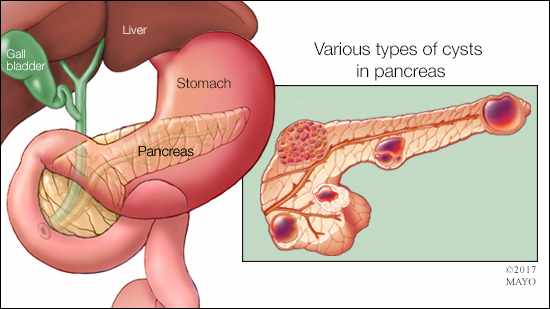
Your pancreas is a long, flat gland in the upper abdomen behind your stomach that makes enzymes and hormones to digest food and process sugar. It is common for sacs of fluid, called cysts, to form on the pancreas, especially in adults over 65. These cysts typically don’t trigger any symptoms. In most cases, they are found during imaging exams, such as CT or MRI tests, performed for another reason.
There are three basic types of pancreatic cysts: those that are not cancerous and stay that way; those that become cancerous over time; and those that have cancer in them when they are found.
Although more than 99 percent of pancreatic cysts never will become cancer, finding one of these cysts causes a great deal of anxiety. Learning there’s a growth on the pancreas — even a cyst that’s likely benign — leads many people to automatically think of pancreatic cancer and how difficult it can be to treat. With that in mind, it’s recommended that when a pancreatic cyst is identified, you meet with a health care provider who specializes in disorders of the pancreas for further evaluation.
The evaluation usually includes a review of your medical history and family history, a physical exam, and an assessment of the cyst’s size, form, structure and location. Small cysts are less likely than larger ones to be cancer or become cancerous. If your health care provider suspects a cyst could be problematic, he or she may recommend additional CTs or MRIs.
When a cyst is large, another imaging exam — called an endoscopic ultrasound — also may be useful. It involves passing a small flexible tube, called an endoscope, through your mouth to your stomach and small intestine. The endoscope is equipped with an ultrasound probe at the tip that enables your health care provider to see an image of your pancreas on a screen. In some situations, an endoscopic ultrasound may be paired with a procedure called fine-needle aspiration that takes tissue and fluid samples from the cyst. Then, those samples are examined in a lab to check if they contain cancer.
Because pancreatic cysts so rarely lead to cancer, the approach recommended most of the time is watchful waiting. Follow-up imaging is performed regularly to monitor the cyst. If it grows or changes in other ways, it may be necessary to drain the fluid from the cyst or remove it completely.
Rarely, a cyst may lead to pancreatitis — an inflammation of the pancreas. When that happens, medication and other treatment often can be used to treat the condition successfully.
If you learn that you have a pancreatic cyst, the best course of action is to consult with an expert who is familiar with these cysts. A thorough evaluation followed by regular monitoring is all that’s needed for most pancreatic cysts. — Dr. Suresh Chari, Gastroenterology, Mayo Clinic, Rochester, Minnesota
Related Articles







