-
Mayo Clinic research uncovers epigenetic roots of digestive disorder associated with diabetes

Living with diabetes can be challenging due to numerous potential complications, including the development of gastroparesis. The digestive disorder, which predominantly affects women, leads to a delay in stomach emptying, causing nausea, vomiting and feeling full.
In a new preclinical study, scientists at the Mayo Clinic Center for Individualized Medicine have discovered insights into the root cause of diabetic gastroparesis. The findings are published in Gastroenterology.
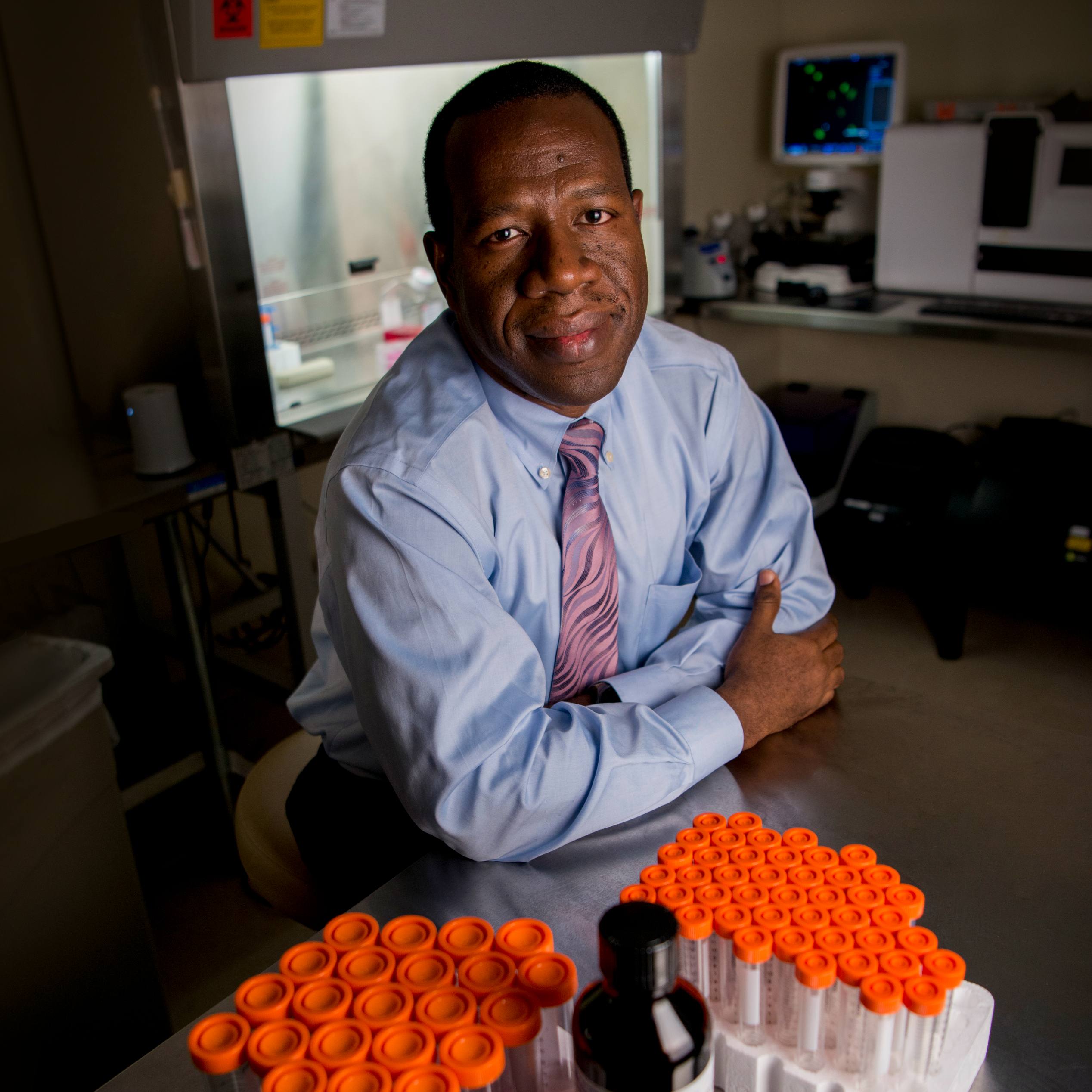
"Our discovery of the underlying epigenetic drivers of gastroparesis has also advanced the understanding of the specific mechanisms the cells rely on when they respond to low oxygen levels that occur in both normal and diseased tissues," says Tamas Ordog, M.D., the senior author of the study and a Mayo Clinic physician-scientist within the Epigenomics Program.
Epigenomics is the study of how genes are turned on and off due to chemical changes in DNA or DNA-associated proteins, without altering the DNA code. These modifications play an important role in regulating the production of proteins, which, in turn, perform essential functions in the body.
Cracking the epigenetic code of gastroparesis
For the study, Dr. Ordog and his team zeroed in on a gene-regulating protein in the gastrointestinal tract called hypoxia-inducible factor 1α (HIF1A), which is known to help cells respond to low oxygen levels. The scientists found that HIF1A is also a key factor in regulating an enzyme called neuronal nitric oxide synthase (NOS1) within stomach nerve cells.
NOS1 in the stomach and intestines produces an important molecule that helps relax the gut wall and widen ring-like muscles to allow contents to be processed and pass between compartments.
Using human tissues from obese diabetic and non-diabetic patients, the scientists found that in people with diabetes, the level of HIF1A in stomach nerve cells responsible for producing NOS1 was notably lower than in people without diabetes. Furthermore, when they removed HIF1A from these cells in female mouse models, it led to a significant decrease in NOS1 and a notable delay in stomach emptying.
As a result of this discovery, Dr. Ordog suggests that targeting H1F1A may be a useful therapeutic strategy.
Next, Dr. Ordog plans to investigate why women are nearly four times more likely to develop gastroparesis than men.
Learn more
Read more stories about advances in individualized medicine.
Register to get weekly updates from the Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information, visit Mayo Clinic Center for Individualized Medicine, or Twitter at @MayoClinicCIM.