-
Mayo Clinic researchers develop new AI tools to reveal seizure hotspots, improve patient care
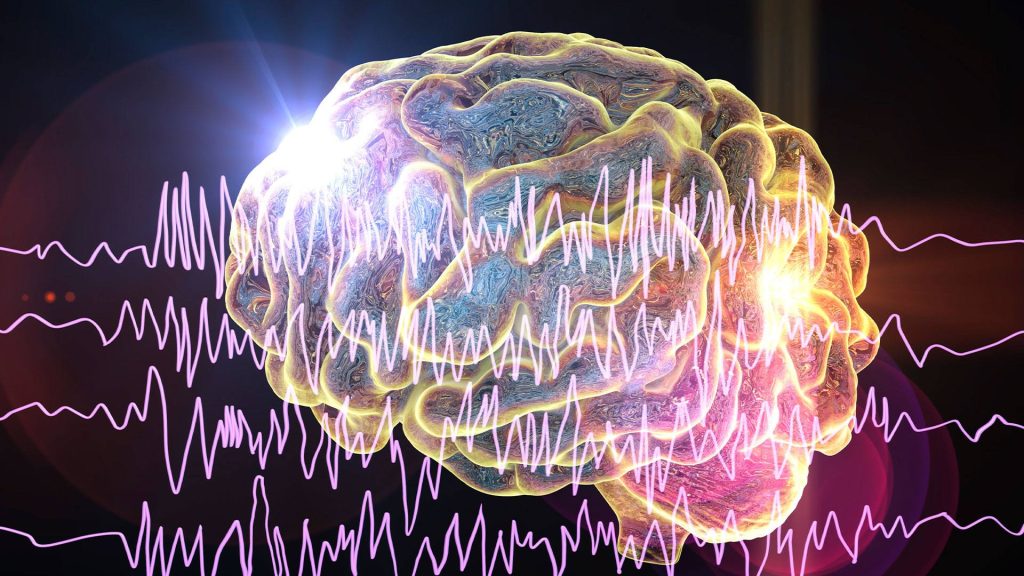
Mayo Clinic researchers have developed new artificial intelligence (AI)-based tools to pinpoint specific regions of the brain with seizure hotspots more quickly and accurately in patients with drug-resistant epilepsy. Their study, published in Nature Communications Medicine, highlights the potential of AI to revolutionize epilepsy treatment by interpreting brain waves during electrode implantation surgery. This transformative approach could significantly reduce the time patients spend in the hospital, accelerating the identification and removal of seizure-generating brain regions.

"This innovative approach could enable more rapid and accurate identification of seizure-generating areas during stereo-electroencephalography (EEG) implantation surgery, potentially reducing the cost and risks of prolonged monitoring," says Nuri Ince, Ph.D., senior author of the study and a consultant in the Mayo Clinic Department of Neurologic Surgery.
Drug-resistant epilepsy often requires surgical removal of the seizure-causing brain tissue. A first step in that treatment is typically a surgery that involves implanting electrodes in the brain and monitoring neural activity for several days or weeks to identify the location of the seizures.
While physicians can detect high-frequency brain waves immediately after electrode implantation, doing so is challenging due to their short duration and low amplitude, as well as environmental noise mimicking pathological events. To detect high-frequency brain waves, they rely on a manual data analysis process that includes visual inspection and artifact rejection to remove unwanted or corrupted data points. This process is labor-intensive and susceptible to error.
Faster, more accurate diagnosis
The researchers developed an AI algorithm that helps pinpoint seizure hotspots, allowing clinicians to make quicker, more accurate decisions about how to proceed.
"We created an AI tool that automatically analyzes EEG recordings during brain surgeries and accurately identifies true high-frequency brain waves associated with the areas of the brain thought to be the source of seizures while eliminating fake high brain waves caused by artifacts," explains Dr. Ince.
Accurately identifying these patterns in EEG recordings helps the healthcare team rapidly find the area of the brain where the seizure originates, enabling the next step: surgery for targeted tissue removal, which is critical for achieving seizure freedom. A faster identification process also reduces the need for prolonged monitoring after electrode implantation. This is essential for minimizing risks, such as infections, which are five times more likely to occur in children than in adults during prolonged stays in epilepsy monitoring units.
The group's future work will focus on transforming the framework into a fully online, real-time system that can interpret the brain waves during electrode implantation surgery and provide feedback to the clinical team regarding the location of the epileptic brain tissue.
"This research could potentially lead to a future where surgical interventions are tailored to individual patients based on their unique brain wave patterns," says Dr. Ince.
Review the study for a complete list of authors, disclosures and funding.
Related Articles