-
Mayo Clinic scientist explains genome sequencing of SARS-CoV-2

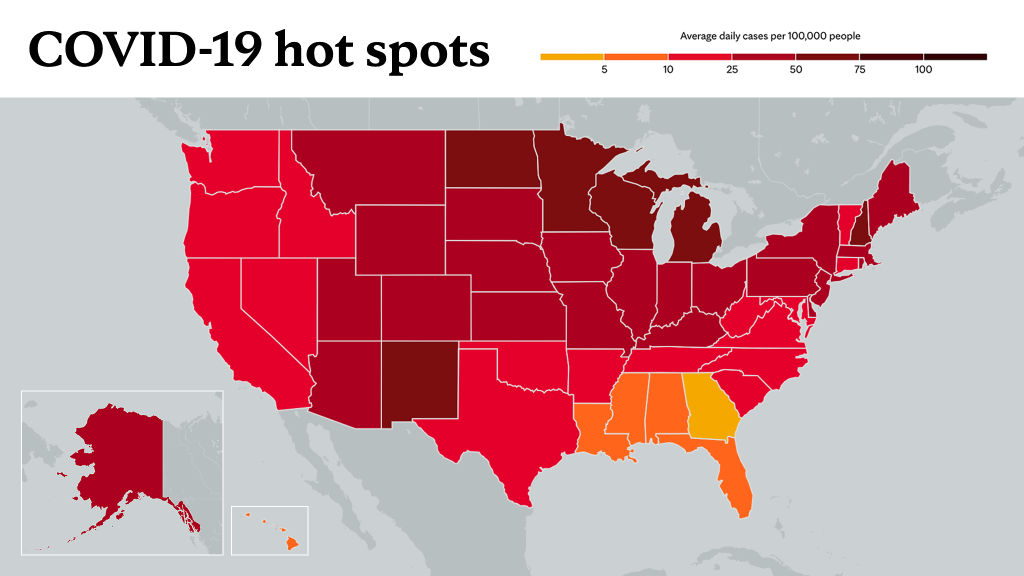
The COVID-19 omicron variant has been reported in nearly half of the U.S. states since it was first detected in California on Dec. 1. The second known case of omicron in the country was identified in Minnesota.
"People that detect omicron — states, counties, countries — that doesn't necessarily mean that they were the first to have it," says Dr. Bobbi Pritt, director of Mayo Clinic's Division of Clinical Microbiology. "It is just that they were one of the first to detect it. In Minnesota, we were one of the first states to detect the presence of the omicron variant. And that's because we sequence a large number of our COVID-19 positive specimens. We have a very good sequencing system in place."
Mayo Clinic Laboratories has been working with Minnesota state health officials and other academic medical centers looking for new variants by analyzing the virus's genetic code.
Watch: Dr. Bobbi Pritt talks about genome sequencing COVID-19 variants.
Journalists: Broadcast-quality sound bites along with b-roll of the Mayo Clinic Laboratory genome sequencing are in the downloads at the bottom of the page. Please courtesy: "Bobbi Pritt, M.D./Microbiology/Mayo Clinic."
To help better understand genome sequencing and how it works, Dr. Pritt answers in this Q&A.
What does tracking a variant or sequencing a genome mean?
When we talk about identifying variants or tracking virus variants, that usually refers to analyzing the viruses genetic code to see if it is a variant and which variant it is.
Can you explain the molecular sequencing process?
First, you have to start with the positive sample. You have a patient sample that contains the SARS-CoV-2 (the virus that causes COVID-19), then you take that positive sample, you subject it to something called extraction where you extract out the virus's genetic code, and purify it, along with all of the human DNA and RNA as well.
Then you subject it to PCR (polymerase chain reaction). And the PCR, in the case of the tests that we're using at Mayo Clinic, are tests that amplify little pieces of the entire virus or nearly the entire virus's genetic code to produce millions and millions of copies. Then all those little pieces that have been amplified need to be sequenced.
Next, the genetic code, letter by letter, is created. And that code is compared to a publicly available sequence library so that you can see if it matches up with one of the known variants or if it might be something completely new.
This is next-generation sequencing — the process of sequencing DNA or RNA by producing millions of sequence reads in a massively parallel manner. Also known as deep sequencing, next-generation sequencing allows for the sequencing of the entire genome of a microorganism.
How is genetic sequencing used for the surveillance of COVID-19 to track these new strains?
You use the information you get from sequencing in a number of different ways to look at what variants are circulating in the community and if there are new variants, perhaps ones that don't even have names yet. That is one of the reasons you would want to sequence is to identify new variants, but usually it's to track the spread of known variants as they go through the community.
What is the time involved and capacity of sequencing machines?
As mentioned above, genomic sequencing is a complex process that involves multiple steps.
Here at Mayo Clinic, we use two different tests for sequencing. One is done in our clinical laboratory and is used primarily for infection prevention and control purposes. The results aren’t used to guide treatment at this point. The other test that we use is done in a research laboratory that has a much larger capacity. We can sequence more than 700 specimens at once. That process takes much longer because we have multiple teams involved.
Why don't all positive tests get sequenced?
Knowing the variant, currently, does not impact treatment, we want to know what's circulating in the community to track how the virus is spreading. By monitoring for variants and sharing information into publicly-available databases, sequencing can help public health officials better understand outbreaks and make decisions.
For instance, if I were to test positive for COVID-19, I'd stay away from other people until a certain time had elapsed, so I knew I wasn't infectious. I don't need to know the variants that I have. But if I was with a group of people and we all got infected, we think at a certain party or event, like what we're seeing in New York City with the anime conference, then it might be helpful to know the variant so we could track the spread from a public health standpoint to understand how that variant may have spread across through multiple people.
What should people keep in mind right now with the new COVID-19 variant?
We need to remember that this is a virus, and it is prone to continue mutating. Some mutations might be clinically important, others may not be at all. A new variant may arise, and then it may go away and it might not ever have any significance. For example, some of the earlier variants — beta, gamma — we don't see those anymore, but the delta variant, on the other hand, did spread very quickly. Keep in mind, whenever we have a new variant, it isn't always an immediate concern. We need to watch and follow its progress over time.
What's most important in stopping this virus and preventing new mutations is to get everyone vaccinated and to continue to use all our preventive measures (wearing masks, social distancing) because the virus only mutates when it's inside of people. The fewer people that are infected, the lower chance that a mutation is going to arise and a new variant will appear.
Everyone should get vaccinated and continue social distancing and wearing their masks. Even though it's tough and we are all tired of the pandemic, we need to remain vigilant.
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a nonpatient care area where social distancing and other safety protocols were followed.
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
Learn more about tracking COVID-19 and COVID-19 trends.