-
Mayo pioneers population science to advance personalized medicine
In a bold move blending pioneering technology with medical science, Mayo Clinic's Center for Individualized Medicine is forging a new frontier in healthcare with the launch of its population omics strategy. This advanced approach uses large-scale "omics" data to connect genomics, environmental factors and health outcomes.
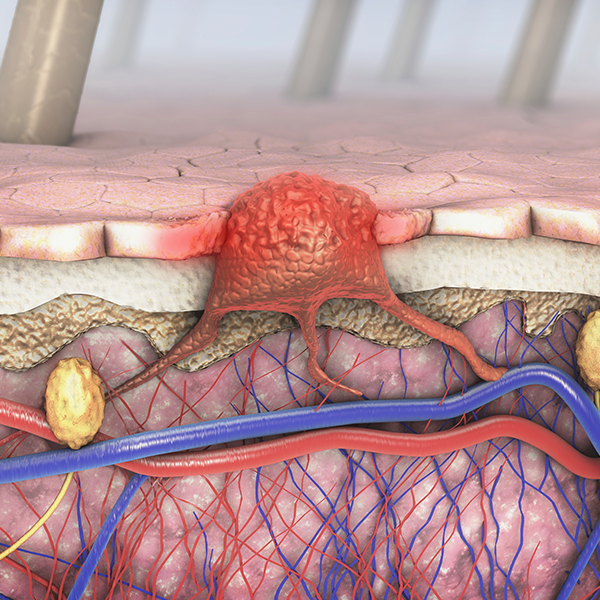
The population omics strategy studies a wide range of biological data from large cohorts — including DNA, proteins, metabolites and more — to uncover patterns associated with diseases. However, these patterns are continuously influenced by environmental factors such as diet, pollutants and microbial interactions, which can significantly alter gene expression and affect health outcomes throughout life.
Omics research drives innovation

To uncover these gene-environment interactions, the population omics strategy dives into new scientific methods that integrate genomics (genes), proteomics (proteins), metabolomics (metabolic processes), transcriptomics (RNA transcripts) and microbiomics (microbes). This research aims to aid multidisciplinary teams in predicting, diagnosing and managing conditions that encompass chronic diseases, aging, inflammatory disorders and cancer.
"Analyzing a diverse set of omics data of thousands of patients can identify novel mechanisms of diseases," says Konstantinos Lazaridis, M.D., the Carlson and Nelson Endowed Executive Director for Mayo Clinic's Center for Individualized Medicine. "Discovering these new paths and eventual targets will allow us to develop innovative interventions to treat diseases."
Targeting hereditary disease risk
Mayo Clinic is piloting the broad implementation of genomic data into clinical use. This family medicine initiative, led by John Presutti, D.O., the Cecilia and Dan Carmichael Family Associate Director for the Center for Individualized Medicine in Florida, offers genomic screening for actionable genetic markers associated with breast and ovarian cancer syndrome, Lynch syndrome and familial hypercholesterolemia, where preemptive interventions may be considered.
The data generated through the screening will be retained for potential future clinical use as part of a comprehensive "genomes for all" effort. As omics technologies advance, the pilot team is evaluating the challenges and potential benefits of using population genomic approaches, considering both immediate and long-term implications.
Exploring polygenic risk scores
Scientists are also developing polygenic risk scores to integrate several genetic variants scattered across an individual's genome to assess their potential for developing certain diseases, like heart and lung diseases, diabetes, asthma and specific cancers. Clinicians will then be able to use these risk scores to potentially customize prevention and treatment strategies.
Polygenic risk scores are supported by advanced genome-wide genotyping and sequencing methods, a robust foundation of research and continued discoveries in links between genes and diseases — all areas where the center has extensive expertise and achievements. Victor Ortega, M.D., Ph.D., associate director for the Mayo Clinic Center for Individualized Medicine in Arizona, says the potential of risk scores is substantial.
"Imagine if you could make informed lifestyle choices and receive screenings to mitigate risk for serious and complex conditions knowing your genetic predisposition for having a heart attack in your 50s, or if you're in the top 5% of the population for the risk of cancer or diabetes." Dr. Ortega says.
As a first step, Dr. Ortega, also a pulmonologist and genomic scientist, is leading the development of a polygenic risk score framework for interstitial lung disease. This condition, marked by progressive scarring of lung tissue, is influenced by both rare gene variants and a collection of more common variants, all of which are captured together in polygenic risk scores.
Artificial intelligence and predicting drug response

One clinical application of population omics involves an innovative artificial intelligence tool, ALMOND (Analytics and Machine Learning Framework for Omics and Clinical Big Data), which was developed by researchers to enhance the treatment of major depressive disorder. This AI tool supports clinicians by analyzing a patient’s genomic data alongside their clinical history, helping them identify patterns that predict how a patient might respond to specific antidepressants.
This support is important as the treatment response for major depressive disorder can vary from one person to another.
"ALMOND exemplifies how population omics can be used in clinical settings to advance personalized drug response assessments by integrating omics data with other clinical and digital biomarkers," says Arjun Athreya, M.S., Ph.D., a computer scientist at the Mayo Clinic Department of Molecular Pharmacology and Experimental Therapeutics, who developed the tool.
Ultimately, the goal of ALMOND is to assist clinicians in tailoring treatments to individual needs, potentially improving outcomes.
Launching the future of medicine
Population omics is designed to integrate new omics methodologies along with electronic health records, enabling clinicians and researchers to collaborate in multidisciplinary teams to advance patient care. It is a key component of a four-part omics strategy.
"These four interconnected omics pillars will accelerate and magnify our impact, drive scientific advancements in individualized medicine and, ultimately, improve patient care," says Dr. Lazaridis. "This ambitious framework underscores Mayo Clinic's commitment to pioneering the omics era so that personalized medicine can benefit everyone."