-
Featured News
Multicenter Study: Multiple Sclerosis Misdiagnosis Supports Improved Education of Clinicians
 ROCHESTER, Minn. – A number of common conditions are mistaken for multiple sclerosis (MS), a disabling central nervous system disease, say researchers at four academic medical centers across the U.S. in a study published online today in the journal Neurology.
ROCHESTER, Minn. – A number of common conditions are mistaken for multiple sclerosis (MS), a disabling central nervous system disease, say researchers at four academic medical centers across the U.S. in a study published online today in the journal Neurology.
While clinicians and researchers have known for decades that MS misdiagnosis is a problem, this study defines the nature of medical conditions that lead patients to be misdiagnosed with MS and possible reasons why they are misdiagnosed. The research involved 24 MS subspecialist neurologists at Mayo Clinic, University of Vermont, Washington University and Oregon Health & Science University, who identified an incorrect diagnosis of MS in 110 patients.
An abnormal response of the immune system, MS causes repeated attacks on the covering around nerve fibers and disrupts communication between the brain and the body, ultimately causing deterioration or permanent nerve damage to areas of the brain, spinal cord and optic nerves. MS is caused by a combination of genes and environmental triggers that predispose to MS.
Unlike some other illnesses, MS has no specific biomarker or blood test. In addition, the related nerve damage can cause a wide range of symptoms, many of which also are often associated with different ailments.
“Misdiagnosis of MS is common; patients may experience common MS symptoms, such as numbness and weakness with a variety of different conditions, many that are more common and less serious than multiple sclerosis,” says the study’s senior author Brian Weinshenker, M.D., a neurologist at Mayo Clinic.
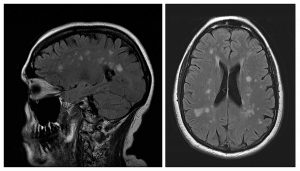
“With the advent of treatments for MS, many physicians feel pushed to reach an early diagnosis, and may be less strict than they should in requiring more specific symptoms or objective neurological findings before making a diagnosis of MS. Nonspecific MRI abnormalities that can mimic those of MS are very common in healthy individuals, and widespread use of MRI as a diagnostic tool increases the rate of misdiagnosis.”
MEDIA CONTACT: Susan Barber Lindquist, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu
In the study, five primary diagnoses or syndromes were identified in two-thirds of participants as the actual causes of symptoms misidentified as MS: migraine, either alone or in combination with other problems; fibromyalgia; an abnormal MRI with unexplained symptoms; a psychological condition; and neuromyelitis optica spectrum disorder, a disease similar to MS that affects the optic nerves and spinal cord.
According to the study findings, 72 percent of the misdiagnosed patients took medication to treat a disease they didn’t have. Some took these medications for many years, and 33 percent remained misdiagnosed for a decade or longer before being evaluated by the physicians participating in the study, who had informed them of an incorrect misdiagnosis. Four of the patients misdiagnosed with MS had participated in clinical trials for experimental MS therapies.
“This study suggests significant and long-term unnecessary risks for these patients,” says the study’s lead author Andrew Solomon, M.D., a neurologist at the University of Vermont College of Medicine.
Some of the treatments for MS carry serious side effects. One drug, taken by 13 percent of the misdiagnosed patients, can cause a potentially fatal brain infection. Other patients suffered from the discomfort and inconvenience of daily injections; others experienced side effects from medications or they lacked treatment for their actual correct diagnoses.
MS diagnostic criteria rely on the accurate interpretation of symptoms, physical exam findings and testing results, such as MRI, to make the diagnosis. The study examined the possible causes for misdiagnosis in the 110 patients in the study and found that the initial clinicians may not have used MS diagnostic criteria appropriately.
“Premature diagnosis of MS should be avoided,” Dr. Weinshenker notes. “When in doubt, physicians often can defer a diagnosis if it is not clear that there is a serious neurological problem or if a patient is stable. Physicians should request a second opinion when they are unsure but concerned that it might be harmful to delay a definitive diagnosis of MS.”
The study identified patients misdiagnosed by both MS specialist neurologists and non-specialists.
“While there may be different reasons for misdiagnoses by subspecialists and nonspecialists, this study suggests that we all make mistakes, and I think we can all do better,” Dr. Solomon says.
Drs. Weinshenker and Solomon say they hope the study will encourage better education of clinicians on the proper use of MS diagnostic criteria and on the problem of MS misdiagnosis, and further study of how to recognize patients incorrectly diagnosed with MS.
Mayo Clinic study co-authors are Dean Wingerchuk, M.D., Brian Rabin M.D.; Michel Toledano, M.D.; W. Oliver Tobin, M.B.B.Ch., Ph.D.; Orhun Kantarci, M.D.; Jonathan Carter, M.D.; and B. Mark Keegan, M.D.
This study is funded by the National Multiple Sclerosis Society PP2074.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, whole-person care to everyone who needs healing. For more information, visit http://www.mayoclinic.org/about-mayo-clinic and https://newsnetwork.mayoclinic.org/.







