-
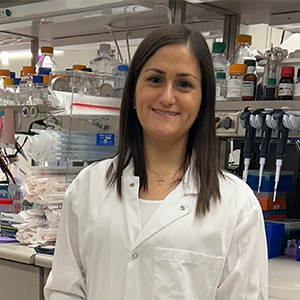
New Mayo Clinic individualized medicine leader on a quest to bring cutting-edge medicine to all

As a pulmonologist and genomic scientist, Victor Ortega, M.D., Ph.D., is leading a charge to breathe new life into precision medicine advancements. His mission is rooted in a deep commitment to health equities and inspired by his grandmother.
"My grandmother died of asthma, and that should not have happened. She was Puerto Rican like me, and Puerto Ricans have the highest severity and frequency of asthma of any ethnic group in the world," Dr. Ortega says. "They also represent less than 1% of people in genetic studies. So, I've made it a life mission to develop cures and diagnostics for people like my grandma, and for all people."
Predicting disease risks: Polygenic Risk Scores
In his new role as the associate director for the Mayo Clinic Center for Individualized Medicine in Arizona, Dr. Ortega is guiding his team toward a transformative future of healthcare, where each person's unique DNA profile may serve as a personalized guide to their health and well-being.
"Imagine knowing your genetic predisposition for having a heart attack in your 50s, or if you're in the top 5% of the population for the risk of cancer or diabetes. With this knowledge, you could make informed lifestyle choices and receive screenings to mitigate that risk," Dr. Ortega says.
Previously inconceivable, he says personalized health forecasts, derived from so-called polygenic risk scores, are possible because of new and sophisticated genome sequencing technologies. The complex scores are compiled from a combination of data from thousands of a person's DNA variants. The data has the potential to predict disease risks, such as heart disease, diabetes, asthma, and specific cancers.
Dr. Ortega says getting to the point where all people know their polygenic risk scores will require a solid foundation of "omics" research and datasets, cutting-edge technologies and further discoveries of gene-disease links — all of which are within his team's expertise and capabilities.
Omics is an emerging multidisciplinary field of biological sciences that encompasses genomics, proteomics, epigenomics, transcriptomics, metabolomics and more.
"It's going to take considerable work and planning, but it really is the way of the future," he says.
Advancing omics beyond research labs
In the shorter term, Dr. Ortega plans to transition more omics discoveries from research labs to the clinic. Omics data can help identify the molecular culprits driving a person's disease, as well as biomarkers that can lead to the development of targeted treatments and diagnostics.
Recent omics discoveries at Mayo Clinic's Center for Individualized Medicine have enabled scientists to predict antidepressant response in people with depression and discover a potential therapeutic strategy for bone marrow cancer. Scientists have also used omics to pinpoint genetic variations that potentially increase the risk for severe COVID-19, uncover potential clues for preventing and treating gliomas and unravel the genetic mystery of a rare neurodevelopmental disorder.
Expanding genomic testing across diseases
Drawing from his years of extensive clinical experience in treating patients with severe respiratory illnesses, Dr. Ortega is also working to expand genomic testing to a broader set of diseases. He highlights the center's collaborative Program for Rare and Undiagnosed Diseases as an effective model that he hopes to amplify.
The Program for Rare and Undiagnosed Diseases proactively engages healthcare teams across Mayo's clinical practice to conduct targeted genomic testing for patients with a suspected rare genetic disease. He says expanding this strategy to more diseases will help build collaborations across Mayo and educate more clinicians on genomics. It may also ensure the most effective genomic sequencing tests are given to patients, ultimately improving patient care and outcomes.
He points to cystic fibrosis, a genetic respiratory disorder, as an example of how genetic misconceptions and wrong testing strategies can negatively affect diverse populations.
"Clinicians might overlook genetic tests for cystic fibrosis in minority groups because of a misconception that cystic fibrosis is most prevalent in people of European white ancestry," he says. "However, the disease can affect various ethnic populations with distinct variants, so they also may order the wrong test."
Clearing the path to cutting-edge medicine for all
Dr. Ortega emphasizes the importance of collaborations and data sharing to accelerate medical discoveries and improve health equity. His dedication to collaborations extends beyond the walls of Mayo Clinic to other consortiums that share profound commitments to enhancing diversity.
"The future of healthcare is happening right now," Dr. Ortega says. "But it's much bigger than genomics advancements and innovations. It's about making sure cutting-edge medicine is accessible to every person."
Learn more
Read more stories about advances in individualized medicine.
Register to get weekly updates from the Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information, visit Mayo Clinic Center for Individualized Medicine, or Twitter at @MayoClinicCIM.

Related Articles