-
 Gastroenterology
GastroenterologyMayo Clinic Health Letter: Highlights from the November 2014 Issue
ROCHESTER, Minn. — Here are highlights from the November issue of Mayo Clinic Health Letter. You may cite this publication as often as you wish. Reprinting is allowed for a fee. Mayo Clinic Health Letter attribution is required. Include the following subscription information as your editorial policies permit: Visit http://www.healthletter.mayoclinic.com/ or call toll-free for subscription information, 1-800-333-9037, extension 9771. Full newsletter text: Mayo Clinic Health Letter November 2014 (for journalists only). Full special report text: Mayo Clinic Health Letter Special Report November 2014 (for journalists only).
New approaches for relief from irritable bowel syndrome
There are new approaches to manage the frustrating symptoms of irritable bowel syndrome (IBS), according to the November issue of Mayo Clinic Health Letter.
 IBS is a common disorder of the large intestine (colon), characterized by abdominal pain that occurs before or along with diarrhea or constipation. Symptoms can vary widely. For many people, flares of diarrhea may last for a few days followed by periods of remission. Constipation may last for days or even months, along with intermittent diarrhea or normal bowel function. A small number of people with severe IBS have unbearable pain that is constant at times.
IBS is a common disorder of the large intestine (colon), characterized by abdominal pain that occurs before or along with diarrhea or constipation. Symptoms can vary widely. For many people, flares of diarrhea may last for a few days followed by periods of remission. Constipation may last for days or even months, along with intermittent diarrhea or normal bowel function. A small number of people with severe IBS have unbearable pain that is constant at times.
Multiple factors may contribute to the bowel dysfunction. The foundation of IBS therapy is developing lifestyle, exercise and diet changes that generally facilitate smooth bowel function. Treatment often includes working with a physician or other care provider to develop a plan for regular exercise and management of stress, anxiety and other psychological factors.
Diet: A doctor or dietitian can offer guidance on identifying and avoiding problem foods and other diet strategies. Increasing fiber intake can help reduce constipation by softening stools, or fiber can help loose stools become more bulky. Recently, experimentation with diets low in certain sugars or in wheat or gluten has come into favor as a possible route toward symptom relief. FODMAP is an acronym for a list of certain fermentable sugars that can be found in fructose or wheat. A dietitian can assist patients with a FODMAP diet that eliminates sugars from diet for a period of weeks to monitor for symptom improvement.
Another approach is related to the recent recognition that some people who don’t have celiac disease may be sensitive to wheat or gluten. A two-week trial of a wheat- or gluten-free diet may be worthwhile for those with mainly diarrhea symptoms.
Nonprescription drugs: When constipation doesn’t improve with diet changes, laxatives such as magnesium hydroxide (Phillips’ Milk of Magnesia) or polyethylene glycol (MiraLax) can be helpful. Anti-diarrheal medication such as loperamide (Imodium) may help, too.
Certain supplements: Peppermint oil in capsules appears to reduce abdominal pain related to IBS. Iberogast is a brand name for a mix of nine herbal extracts that has been associated with reduced abdominal pain with IBS.
Prescription medications: When symptoms are moderate to severe and other changes don’t offer relief, prescription medications may be in order. Drugs to relax the bowel wall (antispasmodics) can be helpful for both constipation and diarrhea related to IBS. A physician may suggest antidepressant medications for their moderating effect on pain perception. For more severe or persistent constipation, the laxatives lubiprostone (Amitiza) and linaclotide (Linzess) may be considered.
New microsurgery techniques reduce swelling from lymphedema
The November issue of Mayo Clinic Health Letter covers new forms of microsurgery for lymphedema that offer noticeable or sometimes dramatic improvements in symptoms.
Lymphedema typically involves the swelling of an arm or leg that occurs when the flow of the lymph system is somehow disrupted. The lymph system includes a network of lymph vessels that help lymph fluid flow into the bloodstream. Cancer treatment, especially breast cancer treatment, is a common cause of lymphedema. It also can develop as a result of damage to the lymph system caused by other cancer treatments or noncancerous conditions.
Sometimes, lymphedema is mild and goes away. Or, it can become a chronic problem requiring diligent physical therapy, various forms of arm and leg compression, and specialized massage and exercise techniques. These measures often keep swelling under control, but not all patients experience sufficient improvements. That’s where new surgical procedures can help.
One procedure is a lymph-to-vein bypass surgery that involves connecting tiny lymph channels in the affected limbs to tiny veins, so blocked up lymph fluids have an outlet to flow into the circulatory system. These connections may be made in multiple locations on the affected limbs during outpatient procedure.
Another option is lymph node transfer. It involves cutting a wedge of skin tissue containing lymph nodes from one area of the body, often the groin, and transplanting into the affected arm or leg. The transplanted lymph nodes are often able to clear lymph fluid from the affected arm or leg, resulting in partial or full reduction in limb swelling. The procedure requires several days in the hospital.
Patients who don’t respond to nonsurgical therapies shouldn’t delay in considering surgical treatment. Continued lymphoma can eventually damage tissues in the affected arm or leg to the point that microsurgery won’t be effective.
So far, these procedures are primarily performed at larger medical centers, such as Mayo Clinic. They aren’t 100 percent effective but they frequently lead to improvements in lymphedema. Usually, the progression of lymphoma halts, and patients can reduce or even stop using compression garments.
Still increasing, but diabetes can be prevented
The incidence of diabetes is on the rise. The November issue of Mayo Clinic Health Letter includes an eight-page special report on diabetes, covering what it is, why it is a serious health concern and ways to prevent and manage the disease.
Report highlights include:
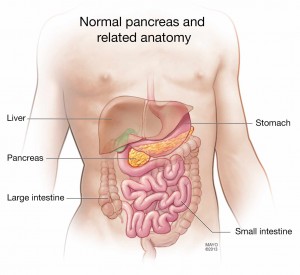
What is diabetes? Diabetes refers to a group of diseases that affect the way the body uses blood sugar (glucose). Too much  glucose can eventually result in serious health issues. Type 1 diabetes occurs when the pancreas makes very little or no insulin. It usually develops in childhood or adolescence. Type 2 diabetes occurs when cells are resistant to insulin made by the pancreas. Insulin is like a key unlocking the door to the cells so glucose can enter. Once the glucose enters cells, the amount of glucose in the bloodstream falls.
glucose can eventually result in serious health issues. Type 1 diabetes occurs when the pancreas makes very little or no insulin. It usually develops in childhood or adolescence. Type 2 diabetes occurs when cells are resistant to insulin made by the pancreas. Insulin is like a key unlocking the door to the cells so glucose can enter. Once the glucose enters cells, the amount of glucose in the bloodstream falls.
Why is diabetes increasing? The rise in the number of Americans with type 2 diabetes parallels the rise in the number of people who are overweight or obese. Excess weight affects the body’s ability to use insulin, leading to insulin resistance. At least one in five Americans has diabetes.
What are the health risks of diabetes? They include heart and blood vessel disease that could lead to heart attack or stroke; nerve damage that can cause debilitating pain, eye damage including distorted vision or even blindness; and foot problems. Untreated, cuts and blisters on the feet can become serious infections. Severe damage might require toe, foot or even leg amputation.
What are the symptoms? The most common diabetes symptoms are excessive thirst and the frequent need to urinate. Symptoms arise from the buildup of glucose. With type 2 diabetes, symptoms tend to develop slowly over a long time. As a result, many people with type 2 diabetes don’t find out they have the disease until they have long-term complications. It’s estimated that 25 percent of people with diabetes don’t even know they have the disease.
What are the tests for diabetes? There are four blood tests available. Any can be used to diagnose diabetes. Adults over age 45 should be tested every three years. People younger than 45 who are overweight and have additional risk factors for diabetes also should be tested every three years. A physician can discuss risk factors that include a sedentary lifestyle, family history of diabetes and being of African-American, Alaska Native, American Indian, Asian-American, Hispanic-Latino or Pacific Islander American descent.
Can diabetes be prevented? A few key lifestyle changes can significantly reduce the risk of developing type 2 diabetes. They center on moderate weight loss through a healthy diet and exercise. A major study known as the Diabetes Prevention Program found that study participants age 60 and older reduced the risk of prediabetes (insulin resistance) progressing to diabetes by 71 percent. To achieve that goal, participants lost 5 to 7 percent of their body weight, ate a healthy diet and increased their physical activities.
It’s never too late to start. Research has shown that older adults seeking to prevent diabetes have better success in achieving exercise and weight-loss goals than do their younger counterparts.
###
Mayo Clinic Health Letter is an eight-page monthly newsletter of reliable, accurate and practical information on today’s health and medical news. To subscribe, please call 1-800-333-9037 (toll-free), extension 9771, or visit http://healthletter.mayoclinic.com/.
MEDIA CONTACT: Brian Kilen, Mayo Clinic Public Affairs, 507-284-5005, Email: newsbureau@mayo.edu







