-
One size does not fit all in benign prostatic hyperplasia treatment
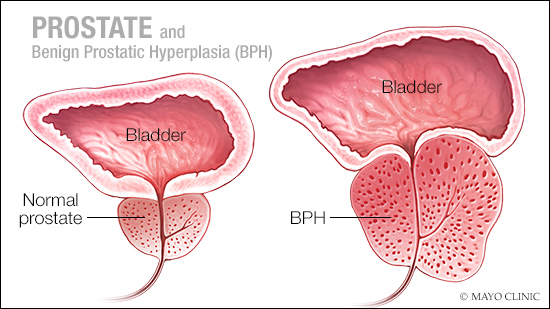 Benign prostatic hyperplasia, or BPH, is a common problem for older men. This condition also is known as an enlarged prostate. With benign prostatic hyperplasia, the prostate enlarges, and the gland presses against, and pinches, the urethra. And the bladder wall becomes thicker.
Benign prostatic hyperplasia, or BPH, is a common problem for older men. This condition also is known as an enlarged prostate. With benign prostatic hyperplasia, the prostate enlarges, and the gland presses against, and pinches, the urethra. And the bladder wall becomes thicker.
An enlarged prostate gland can cause uncomfortable urinary symptoms, including slowing or blocking the flow of urine from the bladder. It also can cause bladder, urinary tract and kidney problems.
Benign prostatic hyperplasia affects approximately half of men over 50 and almost 90 percent of men over 80, according to American Urological Association.
There are various treatments to address benign prostatic hyperplasia, including medications, minimally invasive therapies that use lasers, steam, radio waves and microwave energy, and traditional surgery to remove the overgrown portion of the prostate.
“BPH is not a one size fits all treatment approach,” says Dr. Chandler Dora, a Mayo Clinic urologist. “The right treatment for each patient may depend on many variables, including your symptoms, your urine flow rate, the size of your prostate and your lifestyle. It’s important to review all of those pieces together to make a recommendation for what the best procedure is for each patient.”
Watch: Dr. Dora discusses enlarged prostate and treatment options.
Journalists: Broadcast-quality sound bites from Dr. Dora are in the downloads at the end of the post. Please ‘Courtesy: Mayo Clinic News Network.’
Mayo Clinic is one of the only centers in the Southeast to offer holmium laser enucleation of the prostate or HoLEP surgery. While patients often initially lean toward minimally invasive procedures, many men are surprised to learn that holmium laser enucleation of the prostate surgery provides the most complete removal of prostate tissue of any of the available procedures.
Holmium laser enucleation of the prostate surgery involves inserting an instrument into the urethra and separating the overgrowth from the shell of the prostate with a laser. Then that excess tissue is removed from the bladder. Patients remain in the hospital overnight and require a catheter for 24 hours.
“All treatments for enlarged prostate require catheter placement,” says Dr. Dora. “The amount of time a patient wears a catheter varies from procedure to procedure, so this may be an important factor to consider when deciding which treatment option to pursue.”
Link between benign prostatic hyperplasia and cancer
For some men, elevated levels of prostate-specific antigen or PSA, a protein produced by tissue in the prostate, is often the first indication of an enlarged prostate. When the prostate grows, prostate-specific antigen levels increase. When the entire prostate is removed, these protein levels fall close to zero.
“If a man comes in with an elevated PSA level, it does not necessarily mean that they have prostate cancer. And in fact, PSA is probably a better predictor of prostate size than it is the presence of prostate cancer,” Dr. Dora says.
Nonetheless, it’s important that a man with an elevated prostate-specific antigen be evaluated by a urologist who then can decide whether a biopsy is appropriate, adds Dr. Dora. Increased levels of prostate-specific antigen can occur for men who have undergone partial prostate removal for benign prostatic hyperplasia. Remaining prostate tissue might continue to grow, leading to increased prostate-specific antigen levels, or it could be a sign of infection.
“We take several factors into consideration when deciding on a biopsy: the presence of enlarged prostate symptoms, the size of the prostate estimated on digital rectal exam, and also, very importantly, what we call the PSA kinetics – what was the PSA last year? What was the PSA five years ago?” explains Dr. Dora.
The American Urological Association recommends routine prostate cancer screening for all men 55 to 69.
Men who are at an increased risk of having an aggressive prostate cancer due to a strong family history or African-American men who tend to have more aggressive prostate cancer are encouraged to have a baseline prostate-specific antigen screening prior to age 55.







