-
Preclinical research shows senescent cell removal improves cognitive function
January 27, 2021
Mayo Clinic research findings indicate that the removal of senescent cells in aging mice improves cognitive ability in animals that already show signs of dementia. The results of these tests using senolytic drugs in aging mice appear in Aging Cell.
Senescent cells are those cells in the body that have ignored the order to expire. These cells exist in a suspended state. They are powerful enough to avoid the body's signal to die, but they are not powerful enough to keep dividing. Instead, they linger, spewing out toxic chemicals. The cells and their toxic chemicals often are grouped together as senescence.
Many physical states, such as chronic inflammation, are linked to human cognitive decline. But recent studies also have examined the link between cognitive impairment and senescence. In this paper, Mayo researcher Diana Jurk, Ph.D., member of the Robert and Arlene Kogod Center on Aging, and her colleagues used a two-pronged approach to explore whether cognitive decline can be reversed. One approach focused on the genetic response to a drug ― pharmacogenomics ― while the other examined the problem from the perspective of drug administration ― pharmacologic.

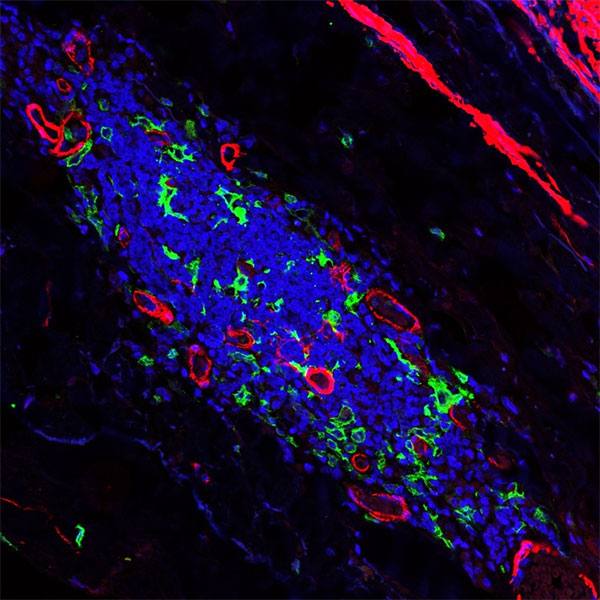
While senescent cells have been previously identified in the brain, it is still unknown which cell types in the brain become senescent during aging. To answer this question, Dr. Jurk and her team used single-cell RNA sequencing, which provides gene expression information from thousands of cells. Using this method, they identified that during aging, senescence is more pronounced in microglia and oligodentrocyte progenitor cells.
They then aged genetically modified mice ― INK-ATTAC mice ― and used two senolytic methods to clear senescent cells: AP20187, which eliminates p16positive senescent cells or the cocktail of dasatinib and quercetin. Both methods significantly improved cognitive function in the mice, based on before and after tests.
The authors write that this finding in mice provides a proof of concept for future studies on senescent cell removal as a potential therapy for age-related cognitive impairment in patients. This finding also reinforced a 2018 Nature paper by Mayo Clinic authors which showed that clearance of senescent cells improved cognitive decline in a mouse model of Alzheimer's disease, as well as previous work by Dr. Jurk and colleagues on senescent cells and anxiety.
Still to be explored are the questions of:
- Mechanistically, how do senescent cells contribute to aging of the brain?
- Which senescent cells were targeted since the therapy was systemic?
- What effect did this intervention have on immune cells in the genetically modified model?
The authors note that additional tests of cognitive function would further validate their findings.
The research was supported by grants from Glenn Foundation for Medical Research, the National Institute on Aging and other National Institutes of Health agencies, the Biotechnology and Biological Sciences Research Council, the Ted Nash Long Life Foundation, The Academy of Medical Sciences, the Conner Group, Robert J. and Theresa W. Ryan, and the Noaber Foundation. The full author list can be found in the Aging Cell article.
- To read more about the toxic chemicals produced by senescent cells, read "Toxic Cellular Ooze Linked to Biological Age, Disease and Disability."
- To read more about aging research at Mayo, head over to The Robert and Arlene Kogod Center on Aging at Mayo Clinic.
- To visualize what's happening in the nucleus of a senescent skin cell, head over to this video, and then come back and read about it in a 2019 article, "Researchers Identify Cells That Drive Human Skin Aging."