-
Q&A with Dr. Limper, the outgoing Robert D. and Patricia E. Kern Associate Dean of Practice Transformation

Andrew Limper, M.D., was the first named associate dean of Practice Transformation, in the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. During his tenure with the center, and through his leadership, Mayo Clinic streamlined practice transformative research and discovery efforts across the institution into a single, unified center. From Dr. Limper's first days on the job, the center's priorities were to innovate and actuate unparalleled patient experience, leverage data and information technology, while integrating care delivery, leading to improved outcomes and lowered costs. And finally, though no less important, to design or redesign systems to enhance staff health and resiliency.
Dr. Limper is stepping down Oct. 1 from the associate dean role after four and a half years at the center's helm. His departure, coinciding with the 10-year anniversary of the Mayo Clinic Kern Center for the Science of Health Care Delivery, offered an opportunity to reflect — both on recent accomplishments and on the unique value the center has brought, and continues to bring, to Mayo Clinic since its inception.
Q: How did the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery come to be?
This is a really great story of philanthropy. We have a long history of innovation at Mayo Clinic, that dates back to the Mayo brothers and Dr. Henry Plummer, also Mayo Clinic having clinical information captured in health records. Mr. and Mrs. Kern were quite interested in using engineering principles — Mr. Kern has a background in engineering — and scientific principles to improve the efficiency and effectiveness of care at Mayo Clinic. In the discussions of Mr. and Mrs. Kern with then President and CEO, Dr. John Noseworthy, the idea came out that we would put together a center that would set a new bar. It would establish new standards for effective and efficient care and work to bring that care out to all people.
I remember sitting on one of the follow-up visits with Mr. Kern and Dr. Noseworthy. Mayo had just passed its 150th anniversary, and Mr. Kern stated that he expected that the center would live on for at least another 150 years into the future to bring that highly effective, efficient care. And so, it was that partnership with philanthropy that brought the center together.
At the end of the day, it's not just about getting the top rankings. It's about delivering the best care for every patient, every day at every door of Mayo Clinic.
Q: How has the work of the center evolved over the years?
The Mayo Clinic Kern Center for the Science of Health Care Delivery was established as a transformational center, coming under both Practice and Research. The goal as a transformational center was to discover new knowledge, and to take new technology and new knowledge and apply them to patient-driven needs within Mayo Clinic's medical practice — to make the Practice more effective and efficient.
In the center, there was broad application of these principles. It wasn't just focused upon a single disease or a single organ. This was quite innovative for a philanthropic gift at that time, to be placed across the Practice — to improve the experience of patients, the health of patients, make it more efficient and reduce the costs upon patients and health care systems.
Dr. Veronique Roger, the first director, recruited fantastic faculty and built a nice center, putting out a lot of innovative work. We became known as leaders in health care delivery. That allowed us to forge collaborations with a variety of partners, including entering into a relationship as a founding member of OptumLabs and building the OptumLabs Data Warehouse — a tremendous resource to understand our practice and to address both research and clinical needs.
Over time Mayo leadership felt there were other groups with overlapping interests. One of the first tasks I was given was to bring these entities together. We were able to expand the center and stretch ourselves beyond our original inception to not only discover new information that would benefit the Practice, but design solutions and then implement them.

Q. You have likened the different capabilities and expertise that comprise the center to three parts of the propulsion of a rocket. Can you explain that?
I actually use the rocket analogy in several ways. It's true that I have looked at our various expertise as each providing one element that boosts our generation of new knowledge. Over time we've morphed our areas of focus. We've increased focus on applied clinical informatics. We've harnessed new tools of data science, including machine learning and artificial intelligence. And as always, health care and health services and outcomes research and our engineering principles. More recently, we're interested in implementation and dissemination science and how we can make the implementation and dissemination of these new solutions better over time. These all provide various types of boosters.
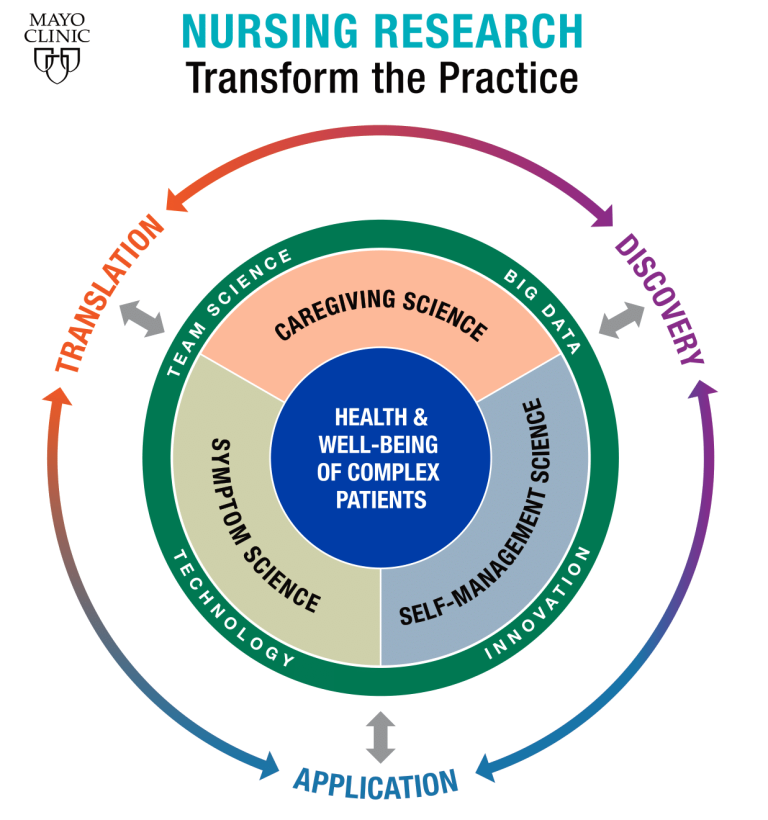
Now the other analogy that I use — which has been used across Mayo — is that there's a continuum in knowledge translation. The first is to Discover — that's often like the research part or the first stage of the rocket. But then we have to not just do that, we have to Translate that information into practice and then ultimately Apply it into practice, thus the three stages of the rocket.
Those are the two analogies that we've used for the center. And it fits very well as we look towards to the future, where we will use new knowledge to Cure. We're going to take that knowledge and Connect with patients, Connect with providers, and then ultimately Transform how we deliver care — the Cure, Connect, Transform, that is part of Mayo's "Bold. Forward." strategy.
Q. As you think back, what are some of the center's most noteworthy accomplishments?
Addressing the opioid epidemic
The center, and particularly Dr. Elizabeth Habermann, led the way on helping to address the emerging opioid epidemic. It was hitting national news, but center-based work helped us to inform where Mayo was at with opioid prescribing and then implement evidence-based prescribing guidelines throughout the Practice. Our work with Mayo's Opioid Stewardship program and partnerships across Mayo, led to Mayo becoming a statewide and also a national voice on this. The center provided great, scientifically-sound evidence on where Mayo was, then scientifically derived guidelines for prescribing, followed by implementation across the Practice for acute opioid prescribing.
Artificial intelligence and clinical trials
The Mayo Clinic Kern Center for the Science of Health Care Delivery has been very engaged in the development of artificial intelligence applications at Mayo Clinic. The center partnering with Cardiology led to one of the first-ever randomized clinical trials to study the use of artificial intelligence in clinical decision support in routine practice, the EAGLE trial, using ECG information to predict cardiac ejection fraction. That was a very exciting pragmatic trial! It serves as a fantastic example of how innovative solutions need to be tested in practice and shown to be of value. It was led by the seasoned research team of Kern Health Care Delivery Scholar alumnus Dr. Peter Noseworthy, and Kern Center health services researcher Dr. Xiaoxi Yao. Pragmatic trials are an emerging tool in that regard. In fact, the Kern Center has recently begun a collaboration with the Center for Clinical and Translational Science to work together to support rapidly conducting and analyzing clinical trials.

Modeling in the pandemic
Of course, over the last 18-20 months, we can't not talk about COVID-19. The center has been quite engaged in COVID. A large talented group led the active COVID modeling work to develop tools that were important both to the Practice — to put the operational plan into practice, but also have gone on to inform state leaders as well as national leaders about where the infection and the pandemic is going, and tracking it as it proceeds and recedes in various parts of the country. Also included with that work are vaccination trackers, planning for personal protective equipment. We have information across all 50 states and we have a very talented group of scientists headed by Drs. Sean Dowdy and Shannon Dunlay — and of course I should mention Dr. Curt Storlie who has led the team for the modeling work.
Setting the stage for innovation and applied informatics
As I came into the center, the applied clinical informatics folks, under the direction of Dr. Steve Peters, were developing a "sandbox," which has become an innovation framework, including information technology and computing tools and infrastructures. It allows early development of artificial intelligence solutions that can add value for the Practice. That's been piloted successfully, through the control tower project for palliative care. We can assess across our hospital practice and identify patients that have serious levels of illness and comorbidities — who would benefit from palliative care consultation. We've seen some very positive outcomes including reduced risk for rehospitalization.
Addressing race, disparities and equity
As we all reflect on the last couple of years, there have been huge issues in racial disparities as well as health care equity. We've been engaged with partners across the board to develop tools to address these issues, including under the leadership of Dr. Renaldo Blocker, raising awareness of inequities for employees of color at Mayo. And we're doing investigations to address issues of health care equity or inequity across Mayo.
Q. What is the center like today?
We're fully embedded within the Practice now — although we still are quite engaged in research. This helps us to focus what we work on. We are there to help inform the Practice, work shoulder to shoulder with our clinical partners to identify problems, often before they become large problems. Discover solutions, test potential solutions. And then when we have solutions that are shown to work, disseminate as broadly as possible.

In that last regard, implementation science is an emerging area. We have to apply evidence as to what various strategies work the best to implement solutions — and then use those interventions to assist in disseminating new solutions to the Practice. The best ideas don't mean anything if we can't deliver them to the Practice and disseminate them across the Practice.
We also know that many of the goals of the center parallel the goals of Quality and Affordability. We have been working closely with Quality, particularly over the last 18 months, and have co-staffed a variety of projects. Going forward, the center along with Quality will report to Mayo's chief value officer, Dr. Sean Dowdy, and his administrative partner in both areas, John Poe. This is of mutual benefit to both entities. The center will bring additional rigorous, scientific-based evidence to Quality and Affordability initiatives. Then those interventions, those solutions, can be disseminated to improve quality measures for all of us.
The newest innovative example of Kern and Quality working closely together in the center is the Science of Quality Measurement program, headed by Dr. Ben Pollock. The measurement of quality parameters and metrics is an emerging science, and incredibly important. This includes both internal standards and public metrics, like the U.S. News and World Report scores and Leapfrog, et cetera. It will help to inform — in a rigorous scientific manner — what is the best way to measure that we are doing a good job? And also inform us of the areas that we need to improve.
At the end of the day, it's not just about getting the top rankings. It's about delivering the best care for every patient, every day at every door of Mayo Clinic. The center and Quality have that same final goal, really, it's the same goal of all of us, which is to deliver ultimate care.
Q. What's next for you?
I have a busy practice in pulmonary medicine with interest in interstitial lung diseases, and I also have a very active research program. I'm going to go back to my practice a bit more, and I'm really looking forward to having more time to do my own research. I do the full extent of research from basic bench research to translational and data science research and also clinical trial work. So, I have some things to finish up and some new ideas I'd like to get launched. I've enjoyed working in the center as much as anything I've done at Mayo Clinic — it's been a great ride! But it will also be an exciting time in this next part of my career, and I'm looking forward to it.
###
Editor's note: This version is excerpted, with updated links and other minor edits from the original article, which was published for an internal audience at Mayo Clinic.
Related link: PubMed listing of opioid-related research mentioned by Dr. Limper.