"Yeah, they're a very complicated surgery," Dr. Rossano says. "You know, prior to the 1980s and '90s, there were essentially no good surgical options for these patients. But a number of very innovative surgical techniques were developed that have allowed many of these children to survive and thrive."
Children born with HLHS go through a series of three surgeries to essentially rework the plumbing of the heart. The first surgery comes within days of birth. The second surgery generally occurs three to six months later. And the third surgery is usually performed about three years later.
This series of surgeries allows children with HLHS to live relatively normal lives, but it isn't perfect.
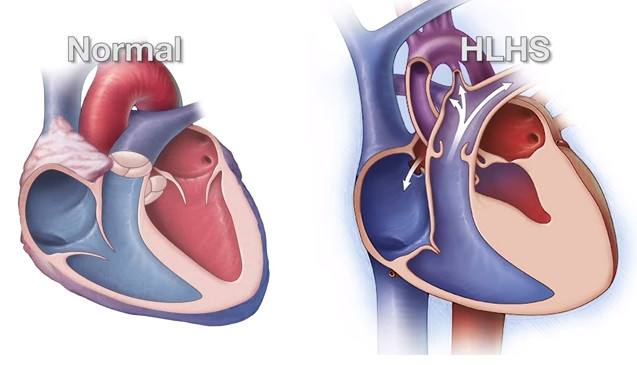
Having the right side of the heart perform the tasks normally handled by both sides of the heart puts tremendous stress and pressure on the right side.
As patients with HLHS are aging, doctors are realizing many of their hearts are unable to continue to function on their own, and some patients need a heart transplant.
But Andrea Sexton found out about a clinical trial going on at Mayo Clinic aiming to solve that problem.
"Quickly they set me up with an interview over the phone with Dr. Nelson," Andrea Sexton says. "He was amazing. He gave me hope."
Dr. Tim Nelson oversees the Todd and Karen Wanek Family Program for Hypoplastic Left Heart Syndrome. He leads a team of roughly 60 people who research and conduct clinical trials for new HLHS treatments.
"The HLHS program has a mission to ... recreate the right ventricle to make it bigger and stronger," Dr. Nelson says. "So we're finding ways of inventing new therapies to make that right heart stronger by stimulating the growth of the heart muscle and make the five-horsepower engine, a 10-horsepower engine, a 50-horsepower engine. And if we make it strong enough, we believe that that has a shot at delaying and preventing transplant for a significant number of these children."
The key to this groundbreaking regenerative therapy clinical trial is stem cells, but not just any stem cells. Dr. Nelson's team uses the babies' own stem cells derived from umbilical cord blood.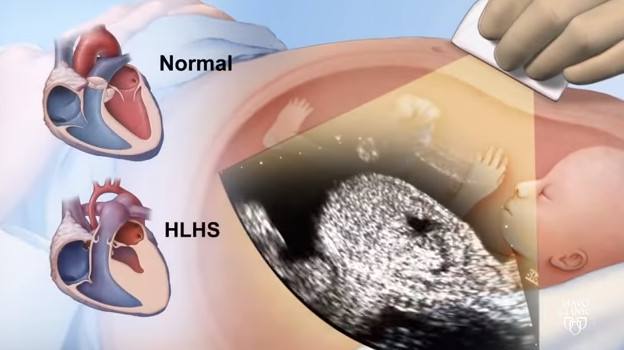
"So the first product that we're testing in our clinical trial is using umbilical cord blood from the baby's own body," Dr. Nelson says. "So the child has to be diagnosed in utero, and we have to be able to collect the cord blood at birth. We can collect the cord blood from anywhere in the country and ship it into Rochester, Minnesota, to have it processed to have a high concentrated product that gets frozen in low temperatures of liquid nitrogen. That product is frozen for three months until the child has their second surgery, or the Glenn operation, which then we can bring those cells back into the operating room, thaw them, and deliver them directly into the heart muscle."
"The hope of this is that it causes a fertilizer type of an effect where these cells are able to fertilize the right ventricle muscle and allow it to grow bigger and stronger because it's received this cell-based therapy," Dr. Nelson says.
On May 4, 2017, Ryals became the fifth clinical trial patient in Mayo Clinic's HLHS team's research.
Dr. Nelson and his team, who had traveled to Philadelphia to deliver the cells, looked on as a surgeon from CHOP injected the cells into Ryals' tiny heart near the end of his operation. A surgical assistant counted down as the surgeon injected the cells into different areas of the heart.
After several tense hours of waiting during Ryals' surgery, his parents were emotional and relieved to hear all went well and that there were no problems injecting Ryals' cells.
During an emotional hug, tears flowed down Andrea Sexton's face as she thanked Dr. Nelson.
"You're welcome," Dr. Nelson says. "He's a trooper."
"I felt like we had a superhero come in on this jet plane, and he had this box of super cells," Heath Sexton says with a big smile stretching across his face. "And it felt like you'd come to save my son."
A few hours later, Dr. Nelson and his team from Mayo Clinic were back on board Mayo Clinic's fixed-wing plane to head back to Minnesota and begin preparations for the next cell delivery in the clinical trial.
In an effort to expand the research and help more families, in 2017 the HLHS team at Mayo began creating a hypoplastic left heart syndrome research consortium.
"So we've built this infrastructure to be able to do clinical trials, and ultimately, we need to be able to have a large number of families participating in that," Dr. Nelson says. "So the consortium really represents our ability to take the science and technology and teams of people to other centers of excellence that allows us to interact with more families at more locations."
CHOP joined Mayo Clinic as the first members of the consortium, and Ryals was the first patient to benefit from it.
Within a few months, Children's Hospital of Los Angelesbecame the third institution to join the consortium, followed soon after by Children's Minnesota.
Dr. Nelson sees the collaboration eventually leading to breakthroughs that once seemed impossible.
"You can even imagine where the technology is leading us – to be able to recreate patches and constructs and maybe even whole ventricles that can be engineered, that can be transplanted at some point," he says.
The days after Ryals received his cells were filled with firsts for the Sextons: a first smile and a first bottle.
They were able to bring Ryals back home to Alabama as a growing, relatively healthy baby boy.
And they finally have what they feared they never would: a sense of normalcy and a chance to dream about Ryals' future.
"I guess I see the survivors of the day that are having children and having careers," Heath Sexton says. "And that's what I see my son as. And the hope is that he can see his grandchildren."
"I see college," Andrea Sexton says. "I see happiness and I see my boys playing together. I see a happy family. And I believe that this work, this research that these doctors have put hard work into is going to – to let us achieve that."
Ryals continues to need minor procedures to maintain the health of his heart. But now, instead of fear and worry filling the Sextons' home, a baby's laughter does.