-
Research finds ethnoracial differences in Alzheimer’s disease

JACKSONVILLE, Fla — A team of Mayo Clinic researchers found Hispanic-American patients with Alzheimer’s tend to survive significantly longer with the disease than other ethnoracial groups, according to a study in Alzheimer's & Dementia: The Journal of the Alzheimer's Association. Hispanic-Americans were found to live an average of 12 years with the disease from the time of the onset of symptoms.
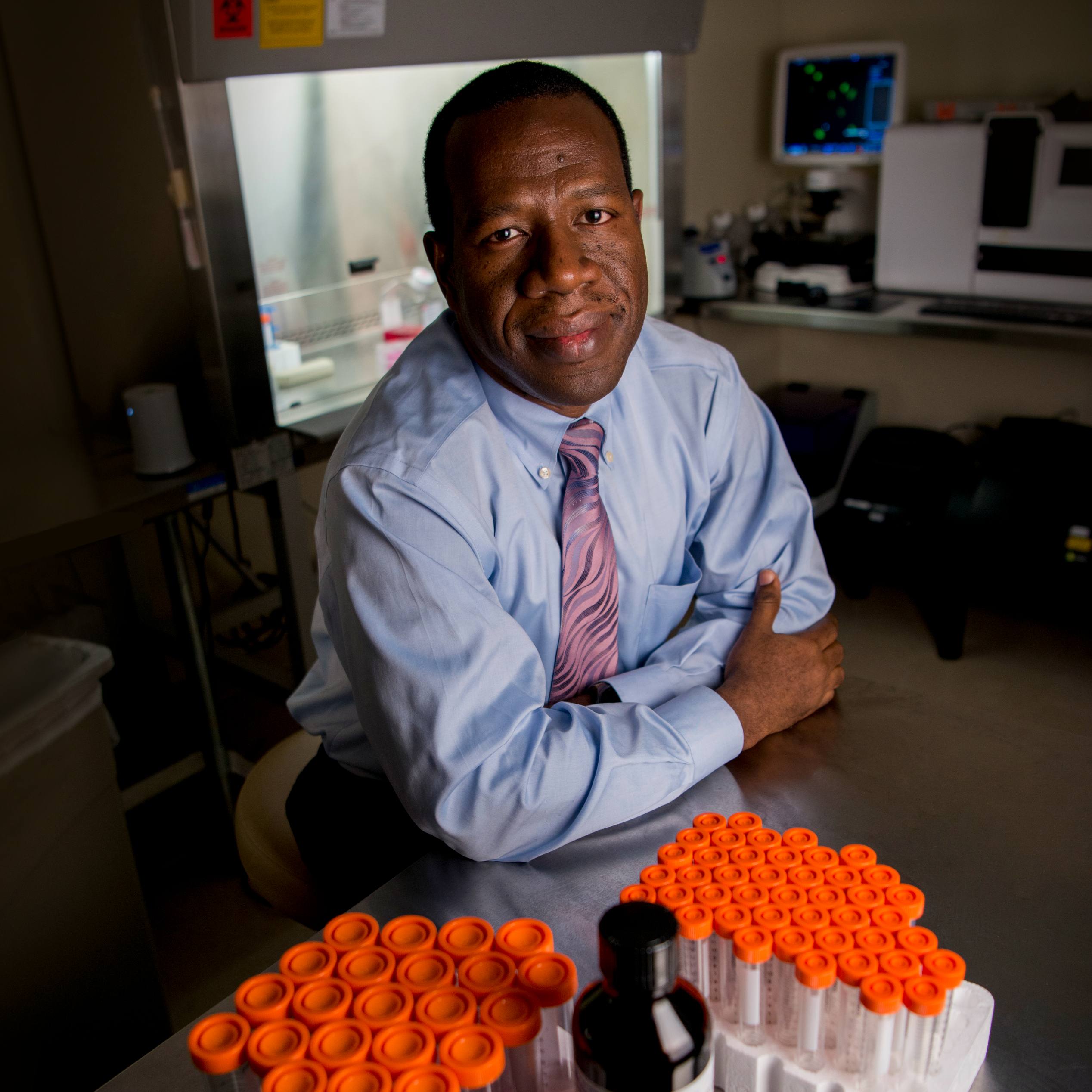
“This study utilized one of the largest series of donated brain tissue to date, looking at demographic and clinicopathologic features of Alzheimer’s disease across an ethnoracially diverse group of cases,” says Melissa Murray, Ph.D., a Mayo Clinic translational neuropathologist and principal investigator on Mayo's Florida campus.
The research team examined 1,625 brain tissue samples and compared the disease progression and duration in individuals who had self-identified as Hispanic, non-Hispanic white, or African-American. Hispanic-American patients had dementia symptoms characteristic of Alzheimer’s at an average age of 70, a year or more earlier than the other groups. They were more likely to have family history of dementia. And they had lower cognitive scores at the end of life. However, the average duration of Alzheimer’s — how long patients lived once they had symptoms — was 12 years for Hispanic-Americans, compared to nine years for non-Hispanic whites, and eight years for African-Americans.
The Mayo Clinic study compared the presence, location and composition of Alzheimer’s-related protein clumps, known as tangles, in tissue samples from the Florida Autopsied Multi-Ethnic (FLAME) cohort. Researchers found subtle differences among the ethnoracial groups in the severity of the tangles, but no differences in brain weight were found. Hispanic-Americans were slightly less likely to have the genetic variant, known as APOE ε4, which is thought to increase Alzheimer’s risk. The study also found distinctions in the distribution throughout the brain of specific Alzheimer’s proteins and the presence of concurrent neurodegenerative processes, which may be relevant to research looking for biomarkers to diagnose the disease.
The study also explored demographic details, such as patients’ education and employment, which are considered to have protective effects against cognitive decline. Compared to non-Hispanic whites, Hispanic-Americans and African-Americans were found to have fewer years of education, which coincides with other risk factors for Alzheimer’s, such as lower socio-economic advantage and increased cardiovascular disease. “As the field works toward Alzheimer’s therapies, ethnoracial differences should be taken into consideration,” says Dr. Murray.
Dr. Murray adds that the study is significant in the size of tissue samples from underrepresented groups. Sixty-seven autopsy-confirmed samples of Alzheimer’s came from individuals who had self-identified as Hispanic. Most described themselves of Caribbean origin, primarily from Cuba and Puerto Rico, while a few were of Mexican, Central or South American origin. The study also included brain tissue samples from 19 self-identified African-Americans. “Hispanic and African- American populations tend to be underrepresented in Alzheimer’s research, despite having 1½ to two times the risk of getting the disease, compared to non-Hispanic white Americans,” says Dr. Murray. “Our hope is that our findings will help Hispanic- and African-Americans overcome the historical and cultural barriers that contribute to their reluctance to participate in research. Our findings of longevity may have important implications in terms of addressing disparities in caregiver needs, social and family impact, and cost of care.”
The findings also prompt the next stage of investigations, looking at factors that may influence survival in Hispanic-American patients, says Dr. Murray. Her team will explore psycho-social contributors, such as family support and potential neuro-biologic factors that include protective proteins.
The study was funded by the State of Florida Ed and Ethel Moore Alzheimer’s Disease Research Program and the National Institute on Aging. Other researchers include Octavio Santos, Ph.D.; Otto Pedraza, Ph.D.; John Lucas, Ph.D.; Amanda Liesinger; Fadi Hanna Al-Shaikh; Kevin Bieniek, Ph.D.; Kelly Hinkle; Owen Ross, Ph.D.; Nilufer Ertekin-Taner, M.D., Ph.D.; Neil Graff-Radford, M.D.; and Dennis Dickson, M.D. — all of Mayo Clinic — as well as Ranjan Duara, M.D., and Maria Greig-Custo, M.D., of Mount Sinai Medical Center in Florida.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, comprehensive care to everyone who needs healing. Learn more about Mayo Clinic. Visit the Mayo Clinic News Network.
- Kevin Punsky, Mayo Clinic Public Affairs, 904-953-0746, newsbureau@mayo.edu