-
Discovery Science
Researchers create ‘mini brains’ to model Lewy body dementia and pinpoint treatments
Lewy body dementia (LBD) is a progressive neurodegenerative disease that shares traits with both Parkinson's disease and Alzheimer's disease but can be more difficult to diagnose. Symptoms can include hallucinations, movement disorders, cognitive issues, sleep problems and depression.
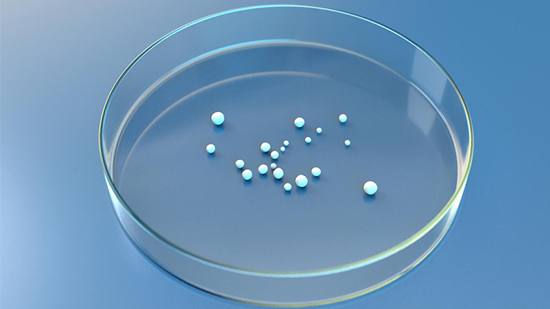
To better understand how the disease develops, Mayo Clinic scientists created mini brain models in a dish that closely match key features seen in the brains of patients with Lewy body dementia. Mini brains, also known as brain organoids, are lab-grown clusters of cells that mimic the human brain structure. The team also identified four potential drug compounds that may offer promising approaches to treating the disease. Their findings are published in Science Advances.
There is no cure for LBD, and scientists say there are few accurate preclinical models available to study it. A hallmark of the disease is a protein called alpha-synuclein, which is encoded by the SNCA gene. This protein is found in nerve cells of the brain and can build up into masses called Lewy bodies, which may contribute to symptoms of dementia.

To better understand the pathology of the disease, a Mayo Clinic research team led by neuroscientist and senior author Na Zhao, M.D., Ph.D., developed preclinical mini-brain models using stem cells from LBD patients who had extra copies of the SNCA gene, which may have caused their condition. The patients donated their skin cells upon diagnosis while they were still alive. Scientists then converted the skin cells to stem cells and used them for research.
Using advanced genomic techniques such as single-cell RNA sequencing, which examines genetic material in individual cells, the researchers showed that their mini-brain models mirrored changes seen in the human brains of LBD patients who had donated their brains to the Mayo Clinic Brain Bank, making the models valuable tools for studying how the disease develops.
The researchers used their novel model system to screen nearly 1,300 Food and Drug Administration-approved drugs, identifying four candidates that may help prevent the buildup of alpha-synuclein in neurons.
"This study suggests that these mini-brain models can effectively mimic disease development, providing a potential platform for testing individualized treatments for patients," says Dr. Zhao. "The four identified drug candidates, which have the potential to inhibit alpha-synuclein and restore the energy production in neurons derived from LBD patients, could be further refined or modified to develop new treatments for LBD and associated dementias in the future."
Researchers say additional studies could introduce additional cell types to better mimic the complexity of the human brain. Researchers could then use these enhanced models to further investigate disease mechanisms, such as exploring how high-risk genes influence the development of LBD.
For a complete list of authors, funding and disclosures, see the paper.







