-
What is the link between Alzheimer’s and Type 3 diabetes?
Researchers have known for several years that being overweight and having Type 2 diabetes can increase the risk of developing Alzheimer’s disease. But they’re now beginning to talk about another form of diabetes: Type 3 diabetes. This form of diabetes is associated with Alzheimer's disease.
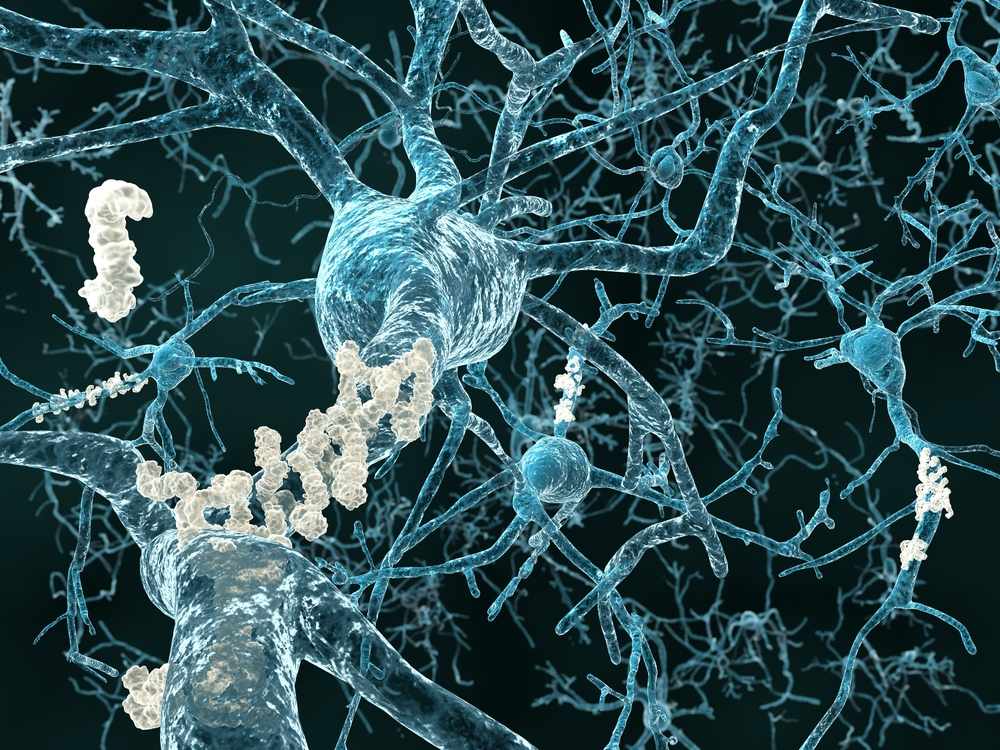
Type 3 diabetes occurs when neurons in the brain become unable to respond to insulin, which is essential for basic tasks, including memory and learning. Some researchers believe insulin deficiency is central to the cognitive decline of Alzheimer’s disease. Mayo Clinic’s Florida and Rochester campuses recently participated in a multi-institution clinical study, testing whether a new insulin nasal spray can improve Alzheimer’s symptoms. The results of that study are forthcoming.
But how is this tied to the Alzheimer’s gene APOE?
A new study from Guojun Bu, Ph.D., a Mayo Clinic neuroscientist and Mary Lowell Leary Professor of Medicine, found that the culprit is the variant of the Alzheimer’s gene known as APOE4. The team found that APOE4, which is present in approximately 20 percent of the general population and more than half of Alzheimer’s cases, is responsible for interrupting how the brain processes insulin. Mice with the APOE4 gene showed insulin impairment, particularly in old age. Also, a high-fat diet could accelerate the process in middle-aged mice with the gene. “The gene and the peripheral insulin resistance caused by the high-fat diet together induced insulin resistance in the brain,” Dr. Bu says. Their findings are published in Neuron.
Watch: Dr. Bu discusses the link between diabetes and Alzheimer's.
Journalists: Broadcast-quality sound bites with Dr. Bu are in the downloads.
The team went on to describe how it all works in the neurons. They found that the APOE4 protein produced by the gene, can bind more aggressively to insulin receptors on the surfaces of neurons than its normal counterpart, APOE3. As if playing a game of musical chairs, the APOE4 protein outcompetes the normal protein and blocks the receptor. APOE4 goes on to do lasting damage to brain cells. After blocking the receptor, the sticky APOE4 protein begins to clump and become toxic. Further, once the protein enters the interior of the neuron, the clumps get trapped within the cell’s machinery, impeding the receptors from returning to the neuron surface to do their work. The insulin signal processing gets increasingly more impaired, starving brain cells.
“This study has furthered our understanding of the gene that’s the strongest genetic risk factor known for Alzheimer’s disease,” says Dr. Bu, who adds that, ultimately, the finding may personalize treatment for patients. “For instance, an insulin nasal spray or a similar treatment may be significantly more helpful for patients who don’t have the APOE4 gene. Patients who have the gene may need additional medications to help prevent cognitive decline.”
Co-first authors of this study are:
- Na Zhao, M.D., Ph.D., Mayo Clinic
- Chia-Chen Liu, Ph.D., Mayo Clinic
In addition to Dr. Bu, other researchers on the team include:
- Alexandra Van Ingelgom
- Yuka Martens, Ph.D., Mayo Clinic
- Cynthia Linares, Mayo Clinic
- Joshua Knight, Mayo Clinic
- Patrick Sullivan, Ph.D., Duke University School of Medicine
- Meghan Painter, Ph.D.