-
Rural Women Less Likely to Get Radiation Therapy after Lumpectomy for Breast Cancer
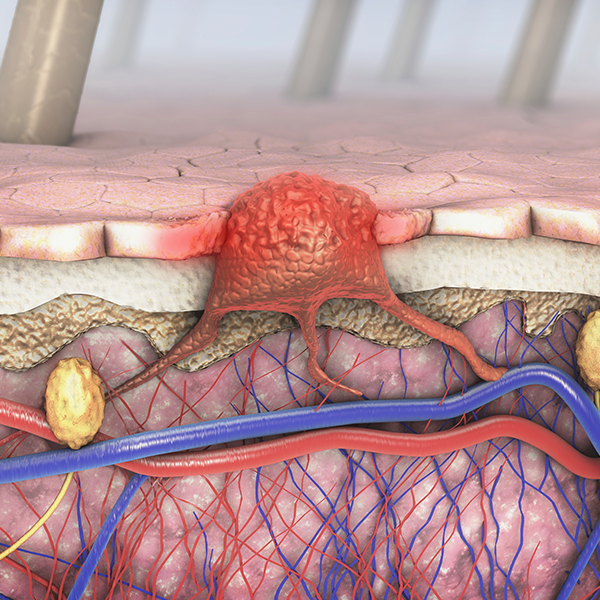
Rural women with breast cancer are less likely than their urban counterparts to receive recommended radiation therapy after having a lumpectomy, a breast-sparing surgery that removes only tumors and surrounding tissue, a study by Mayo Clinic and others found. The difference is one of several rural disparities in breast cancer diagnosis and treatment the researchers discovered. The findings are being presented at the AcademyHealth Annual Research Meeting in Baltimore.
MULTIMEDIA ALERT: Multimedia resources are available for journalists to download on the Mayo Clinic News Network.
"These study results are concerning," says Elizabeth Habermann, Ph.D., associate scientific director, Surgical Outcomes, Mayo Clinic Center for the Science of Health Care Delivery. "All women should receive guideline-recommended cancer care, regardless of where they live."
Using the 1996 – 2008 California Cancer Registry, researchers at Mayo Clinic, the University of Minnesota and Georgetown University analyzed the care given to nearly 350,000 urban and rural women with all stages of breast cancer. Although there were no significant mortality differences between the two groups, researchers found that rural women were less likely to have their estrogen receptor status tested and their tumor graded — two important elements of the diagnostic work-up for breast cancer.
In addition, rural women were also more likely to choose mastectomy — complete removal of the breast — than lumpectomy. Rural women choosing lumpectomy were less likely to get the recommended radiation therapy following surgery, the study found.
"The lumpectomy findings are worrisome because lack of follow-up radiation therapy could lead to recurrence, another surgery, and another time period of concern for the woman and her family," Dr. Habermann says.
The researchers recommend further research to determine why rural women are less likely to choose breast-conserving therapy and get recommended cancer diagnosis and treatment. Interventions then can be designed to address the gaps, they say.
Co-authors include Christopher Chow, M.D., University of Minnesota; Waddah B. Al-Refaie, M.D., Georgetown University Hospital; Wei Zhong, Ph.D., Genentech; and Judy Boughey, M.D., Mayo Clinic.
The study was supported by National Institutes of Health grants HL65176 and NIH 1 UL1 RR024150.