-
Research
Science Saturday: Blood Tube Optimization Program hails first successful project

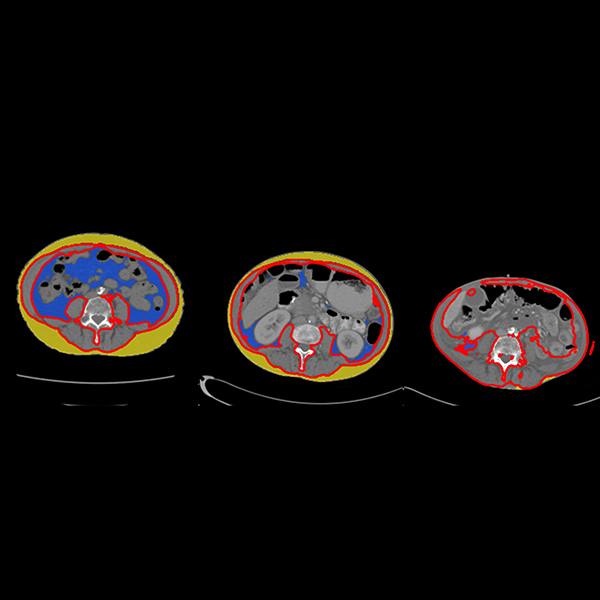
Frontline staff in the Central Clinical and Central Processing Laboratories in the division of Clinical Core Laboratory Services (CCLS) made an astute observation that more tubes of blood were being collected from patients than seemed necessary. Analysis pointed to a potential benefit of new laboratory automation equipment and technology. The previous automation line in Central Processing required all tubes loaded in a rack to be the same height and serum aliquoted into cups for testing. The new automation line can accept varying tube sizes/heights and sends tubes directly to the analyzer, which reduces the amount of blood needed for testing. The lab teams seized this opportunity to make a change.
Intent on improving the patient experience, realizing supply efficiencies, and achieving cost savings for the enterprise, the lab teams enlisted the sponsorship of Drs. Nikola Baumann, Darci Block, Matthew Binnicker, Brad Karon, and administrative sponsors Adi Singh and Tim Faber. Together, an operational excellence goal emerged.
The team moved forward with its first pilot involving updating the collection and roll-up of blood volumes for 111 CCLS Rochester tests. A recent go-live on Feb. 20 included 94 test updates. Based on the post-go-live data, the results equate to a 59% decrease in blood volumes collected, which would be 1,071L/283 gallons reduction annually. Considering that the average human body has about 1.3 gallons of blood, the effect of this improvement is immense.
There was a corresponding 41% decrease in SST tubes for this project. That’s 2,891 fewer tubes per week, or $24,076 cost savings per year. No adverse effects to “quantity insufficient” (QNS), redraws, or add-ons have been detected. This not only benefits patient safety and satisfaction because less blood is collected but also conserves blood collection tubes and reduces supply chain demands.
The project evolved quickly into a program. With dedicated support, the team is forming cross-divisional partnerships across the enterprise to bring forward project ideas and pilots, all focused on blood and tube optimization. The benefits? Not only is there potential for greater patient safety and satisfaction and supply conservation, but fewer blood tubes might reduce the potential for manual errors in labeling and sample mix-ups and reduce the load on the overall system. Fewer tubes also have the potential to improve test turnaround time.
This first project is just the beginning and is considered proof of concept. There are four more projects currently getting started in the program.
Special thanks to the efforts of so many, but in particular: Dr. Binnicker, Dr. Baumann, Dr. Block, Dr. Karon, Adi Singh, Tim Faber, Sherry Boedecker, Sam Crosby, Elaine Elliott, Erin Hain, Brenda Hendrix, Sharon Johnson, BJ Krekelberg, Sara Minnich, Ryan Nett, Aaron Stelpflug, Jennifer Storlie, Chris Yoch, the Lab Test Catalog Team (Karen Kloke and Kristina Erath Pike), and the Test Implementation Service Team (Maxwell Cain, Shanna Hanson, Sean King, Melissa Rivera, Ryan Ritzer, and Kimberly Smalley).
____________________________________________
Mayo Clinic medical research websites:
- Research at Mayo Clinic
- Discovery’s Edge
- Mayo Clinic Laboratories
- Center for Individualized Medicine
- Center for Regenerative Biotherapeutics
- Center for the Science of Health Care Delivery
- Mayo Clinic Comprehensive Cancer Center