-
Research
Science Saturday: Good Advice on Obesity? Wait for it…
With obesity, good advice only goes so far. What’s good for one person hasn’t turned out to be good for all, and it’s left patients and physicians adrift. Michael Jensen, M.D., a Mayo Clinic endocrinologist, began studying obesity 34 years ago when it seemed manageable.
“There was sort of a false sense of optimism,” says Dr. Jensen. “Now the problem is so prevalent and doctors are so pessimistic that they just tend to not address it at all.”
Dr. Jensen, who wears running shoes with his suit, stops his treadmill desk and heads to his office filled with binders covering the hundreds of studies he’s managed over the decades. His research is a fraction of the whole. The level of obesity research has doubled nearly four times since 1996. But the massive collection of data hasn’t stopped this epidemic. Andres Acosta, M.D., Ph.D., a Mayo basic-science-trained gastroenterologist who is board-certified in obesity medicine, describes the numbers.
“Almost 600 million people suffer from obesity across the world. In the United States alone, 40% of people have obesity. And despite FDA-approved medications, devices and surgery, less than 1% of the patients ask for them,” he says. “We also have a new diet every week and a new weight loss program every week. All of them secure weight loss, none are effective in the long-term. So that's a reality of obesity.”

Dr. Acosta and Dr. Jensen are not alone. Across Mayo, hundreds of researchers from the bedside to the lab are delving into obesity starting at its very core: the very active and dynamic tissue we call fat.
Fat goes from fuel to driver
“This is extremely controversial, but this is the way we’ve decided to tackle this problem,” says Dr. Acosta. “Obesity, despite whatever people say, is still a disease of energy balance: what we eat versus what we burn.”
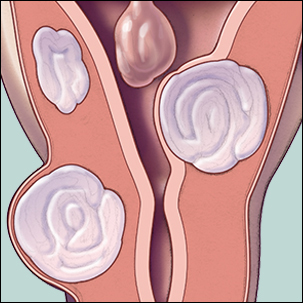
Get out of balance, he says, and we start to gain weight or store fat, and it’s that fat which causes the problems. Fat tissue used to be considered just fuel. It provided for the body in case of nutritional turbulence, and that’s true at the most basic level. “The average, normal weight woman probably can store the caloric equivalent of three months of ‘groceries’ in body fat and take it out when it’s needed,” says Dr. Jensen. Even looking at fat cells gives you that idea. Their most striking feature is a giant reservoir containing a triglyceride (similar to cooking oil) with the cell’s nucleus and organelles squished in where there’s room. The fat cell’s main job is to remove excess fat from the bloodstream, hold it safely and then release it back out when the body needs it. The process is highly controlled. Fat cells pay attention to their own internal status, their habitat, their neighbors and information coming in from around the body in order to do their job.

“Fat cells are about 95% fat and do just fine because they have mechanisms to control it,” says Dr. Jensen. “But the other places that fat can be stored, like in the liver, those other cells are much, much less able to store it safely.” In cases of fat overload or non-triglyceride forms, fat molecules can have a toxic effect on cells, interfere with insulin efficiency or actually generate signals that cause cells to die.
“Imagine a pool filled with thousands of gallons of water,” says Dr. Jensen. “A normal functioning fat cell would be like a pool filter set to release one teaspoon a minute. Now imagine that the filter accidentally releases 1.4 teaspoons a minute. That’s the difference, over time, between healthy and diabetes.”

Fat cells that are poorly regulated don't respond to the normal signals, says Dr. Jensen. For example, when a person doesn’t eat for a certain period of time, the stomach cranks up appetite using ghrelin, a molecule called the ‘hunger hormone’ because it causes your appetite to increase. Ghrelin is released from the stomach, enters the bloodstream and crosses the blood brain barrier to prod your grey matter into action. At that point you start thinking, wouldn’t sushi be good? Metabolic action complete.
Resetting Receptors
In addition to appetite, though, ghrelin is also involved in the physical processes associated with cravings and addiction. As part of his research into cocaine addiction, Stephen Brimijoin, Ph.D., a Mayo Clinic neurobiologist, began studying ways to offset the high of cocaine by altering the enzyme butyrylcholinesterase.

During those studies, Dr. Brimijoin and his colleague, Peng Chen, Ph.D., found that their altered enzyme also lowered levels of ghrelin. So the researchers are beginning to look at the altered enzyme’s effect on one obesity-related challenge: yo-yo dieting. After cycles of weight gain and loss, ghrelin receptors in the brain do not work correctly. The body needs gentle appetite nudges, but the ghrelin pathway is set to punch. That translates into an urge to eat more than the body needs. To reset the receptors, the revved-up enzymes deplete the excessive ghrelin, resensitizing the brain receptors to the amount of the hormone that remains. Their work, published in Frontiers in Pharmacology, continues with help from many sources, including the group Regenerative Medicine Minnesota.
Tuning the Antennae
Fat cells also react to their habitat. One way they do that is through antenna-like structures, called “cilia.” When cilia fail to work correctly, their dysfunction gives rise to a range of diseases. Those genetic disorders, such as Bardet-Biedl syndrome, sometimes include obesity as part of their presentation. A team led by researcher Jinghua Hu, Ph.D., is examining a specific protein associated with the function of cilia, called FBF1. In a paper published in Nature Communications in 2016, the team reported that FBF1 plays a key role in the gate that forms between the cell and cilia. In terms of obesity, their theory is that shutting that gate, or depleting FBF1, could prevent cells from directing fat into other cells, such as those in the liver or muscles. They expanded on these findings in 2018, suggesting a new target for investigation. While tangential to obesity that isn’t related to ciliopathies, the team hopes this approach could help those with ciliopathies or with certain metabolic disorders associated with obesity in general.

Retraining Fat to Burn
The complexity of fat cells extends even further. Instead of just one type of fat cell, there are two. Fat cells, also called adipocytes, come in two varieties: white and brown. White adipocytes store fat in one large droplet and release fatty acids for other tissues to use, say for hormones. Brown adipocytes have many smaller droplets of fat and use it to generate heat. Researchers have found, however, that with long-term exposure to cold temperatures, some adipocytes look white but act brown. These beige or “brown in white” (brite) adipocytes are thought to shift due to a protein called “fat-specific protein,” or FSP27. By understanding how FSP27 manages to change the action of white adipocytes, researchers hope to identify pharmaceutical interventions to help people lose weight. A team led by Jun Liu, M.D., Ph.D., received a Mayo Clinic Center for Biomedical Discovery award to study FSP27, and their latest publication looks at the effect of bariatric surgery on FSP27 expression in an animal model. Since many people managing obesity opt for surgery, this type of research helps understand how that intervention works at a cellular level.
Ultimately, basic research into fat cells and how they communicate, respond to the body and do their job helps generate the next generation of drugs, devices and surgeries to treat obesity.
But new treatments are only part of the story. People are the other part.
People and artificial intelligence for the win
Often, says Dr. Acosta, his patients don’t know their obesity can be treated. He says too often people focus on how severe their body mass index is, instead of why that person has obesity. To find the cause, Dr. Acosta and his team, in collaboration with his mentor Michael Camilleri, M.D., are taking a new approach.

They collected data on a variety of well-validated measures from animal and human trials, and gathered that information for 509 patients across the obesity spectrum.
“We then asked the computer, ‘How would you classify obesity if you have these variables in these patients?’” he explains. The computer told them:
- Hungry brain: Patients don’t feel full so they eat a lot of calories
- Hungry gut: Patients feel full at first but within an hour or two feel hungry again
- Emotional hunger: Patients eat for reward, either for a good day or for getting through a bad day
- Slow burn: Patients who burn fewer than expected calories
Dr. Acosta and his team think that patients are evenly distributed between the classifications with some overlap, and there are some people who don’t fit into any of the categories. But for those who have received a research protocol designed for their classification, the team has shown that weight loss is greater than when patients receive standard care.
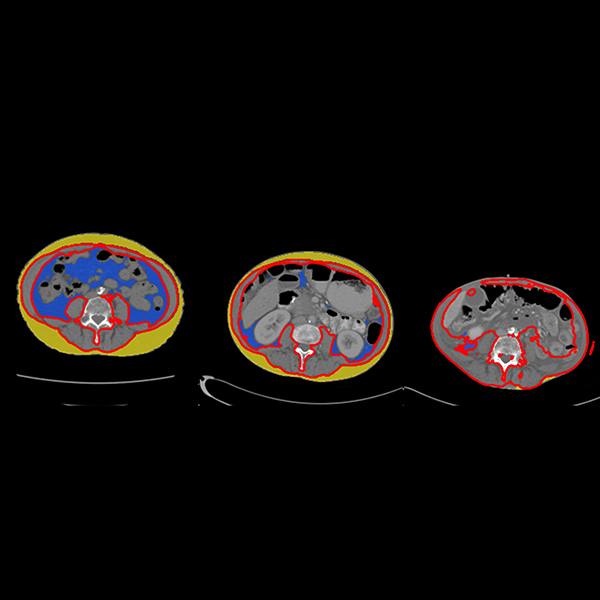
“We are bringing precision medicine to the management of obesity,” says Dr. Acosta. But that precision comes with a cost. To identify a person’s classification, the volunteer spends two days in Mayo’s clinical research unit. They give blood, stool, saliva and DNA samples. They’re scanned to measure fat mass and tested to see how fast their stomach empties. After all that, four hours of questions.
Not practical for a primary care visit.
So, armed with the data from the study, the team is now validating its classifications and searching for a telltale fingerprint to make the process less intrusive.
“If we can simplify obesity with a blood test and offer a treatment algorithm based on phenotypes, we can move the dial on this disease,” says Dr. Acosta. That, he says, would have a cascade of effects.
“Most times physicians will treat the diabetes, the hyperlipidemia, the hypertension, joint pain, the sleep apnea, the stroke, the depression, anxiety, the cancer, liver disease, the gastric reflux, but they ignore the cause: obesity,” he says. “It’s one treatment instead of 14 pills. But they don’t have the tools.”
What Dr. Acosta’s team, supported by Mayo's Center for Individualized Medicine and the Center for Biomedical Discovery, is doing now is identifying new targets with single cell RNA sequencing, which examines the RNA instructions within a specific type of cell, and using multiomics — which combines information from our genome, microbiome and other “omes” — to dig deeper into the phenotypes and identify new treatment possibilities.
“We need the basic science information to understand how the target works and compounds that might be an option for the new protein, molecule or whatever so we can bring it back to the bedside,” says Dr. Acosta.
And not a moment too soon.
“People with obesity are more likely to die from obesity,” says Dr. Acosta. “And if we put that in years and we compare someone with obesity versus someone who does not have obesity, they will live 13 years less. So obesity matters, for many of us.”
The good news is that fat tissue is getting the attention it deserves. Discovery research in the lab and the clinical setting is contributing new information on both fat and obesity. And there’s a lot more to come. Researchers are aiming for no less than the Big Bang Theory of obesity. “There's been a lot of great work done, but I wouldn't say there's that unifying theory,” says Dr. Jensen. “Yet.”
After 34 years, it’s just getting interesting.
- Sara Tiner, November 2019
Mayo Clinic and Dr. Acosta have a financial interested related to a technology referenced in this article.