-
Science Saturday: Link found between key gene and two neurodegenerative diseases
Gene expression can amplify the risk of neurodegenerative diseases for patients, but researchers are still figuring out which genes have an outsized effect on risk and why. In a new paper published in Nature, Mayo Clinic researchers and collaborators have zeroed in on variants of one gene critical for nerve cell function that ups the ante for patients with Lou Gehrig's Disease, also known as amyotrophic lateral sclerosis (ALS), and frontotemporal dementia (FTD).
"This finding helps clarify a new direction for biomarker research and provides a therapeutic target for ALS and FTD research," says Yuka Koike, M.D., Ph.D., a Mayo neuroscience fellow, and one of the lead researchers in the study.
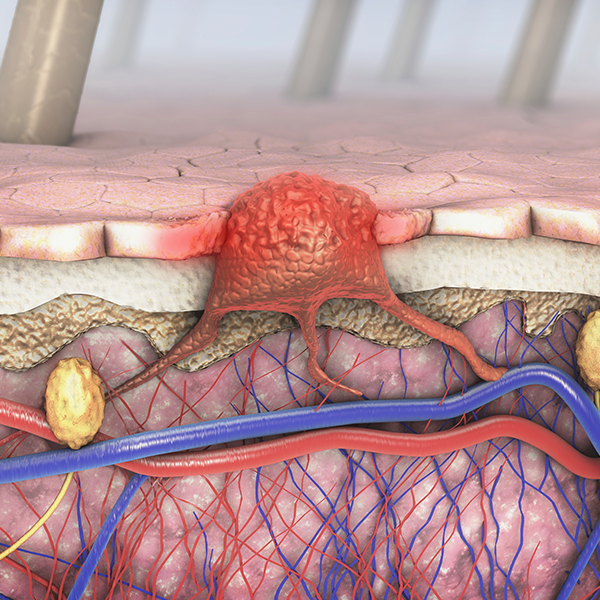
In the nucleus of brain neurons, the protein TDP-43 helps prepare RNA “instructions” used to make proteins that cells need for proper functioning. TDP-43 is like a copyeditor, looking for typos in a block of text. Without it, messenger RNA contains errors that lead to faulty protein assembly and, potentially, to disease. For example, without TDP-43, a messenger RNA “typo” is linked to sporadic and inherited cases of ALS.
Researchers from Mayo Clinic, Stanford University School of Medicine, and other collaborating institutions wondered if there were more examples of typos that TDP-43 corrected.

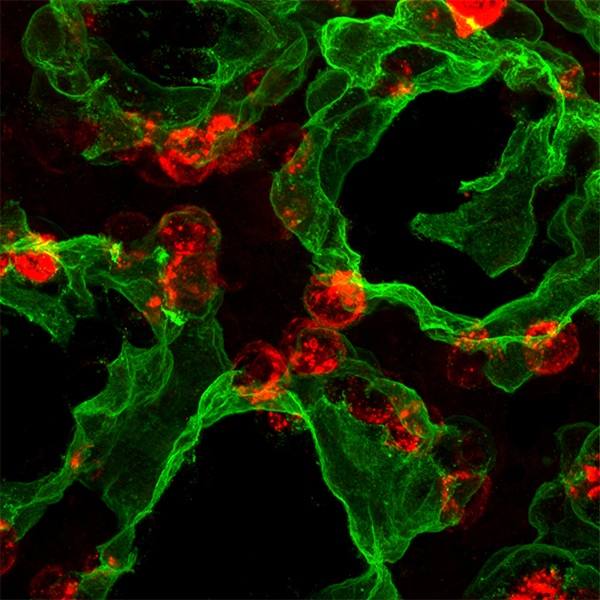
To find out, they started with brain tissue samples donated by patients with ALS and FTD. The team compared the RNA instructions to see what proteins would be made in neuronal tissue samples with TDP-43 and those without the protein. They found various genes that were activated or expressed at different levels. The effort identified 66 gene alterations – two that have been verified previously as targets for TDP-43 copyediting – but one that was a surprise. Called UNC13A, this ALS-FTD risk gene is part of a gene family that makes proteins for the nervous system. These genes got their name because animals with mutations in these genes have uncoordinated movements due to neuronal defects.
Without TDP-43, the instructions for UNC13A contain ‘typos’ that result in less of the protein coded for by the gene – which is a problem for neurons. The scientists also found that variants of UNC13A with more errors were associated with decreased survival in patients. They propose that UNC13A alterations are present in the genetic “text” and when TDP-43 stops copyediting, the UNC13A errors contribute to the development of ALS and FTD.

"Variants in UNC13A are one of the most commonly identified risk factors for FTD and ALS in genetic studies, but up until this time, it was unclear how these genetic variants resulted in increased disease risk," says Leonard Petrucelli, Ph.D., co-senior author of the paper. "Identifying the pathology in this gene upon TDP-43 loss was therefore particularly exciting. Our data helps us to finally gain a better understanding of why UNC13A is an ALS and FTD risk gene." Dr. Petrucelli is a Mayo Clinic molecular neuroscientist and the Ralph B. and Ruth K. Abrams Professor of Neuroscience.
"If these gene variants can be detected in patients' biofluids, they could act as biomarkers for FTD and ALS, potentially allowing us to generate tools that help with disease diagnosis and predict individual disease severity," says Mercedes Prudencio, Ph.D., a neuroscientist and one of the lead researchers on the study. "Further, identification of genes and proteins that are relevant to the disease process can direct research towards understanding the specific molecular changes that happen in diseased cells and help us develop effective treatments."
The research was funded in part by NIH grants. For a full list of funding, disclosures, collaborators and authors, including co-senior author Aaron Gitler, Ph.D., from Stanford University School of Medicine, see the paper.
— Lynda de Widt, March 9, 2022