-
Science Saturday: Research News Roundup — September 2018

Each month, we publish Mayo Clinic's Research News Roundup. This article includes brief summaries and links to news releases from the preceding month that discuss some of our latest medical research. It also connects readers to related resources.
Read on for recent findings of Mayo Clinic Research:
A team of researchers from Mayo Clinic Cancer Center has been awarded a five-year, $11.5-million Specialized Program of Research Excellence (SPORE) grant in liver and biliary tract cancer from the National Cancer Institute (NCI).
Specialized Program of Research Excellence grants are designed to promote interdisciplinary research and help basic research findings move quickly from the laboratory to patient care.
To earn these competitive grants, institutions must demonstrate a high degree of collaboration between top scientists and clinicians and show excellence in translational research projects.

The medical community has long known that patients on long-term opioid therapy often have significantly more health care visits. But adhering to a standardized care process model for opioid prescriptions appears to reduce the overall number of health care visits for these patients while maintaining safety, shows new research published in Mayo Clinic Proceedings.
Controlled substance agreements outline an individualized pain care plan for patients ─ in this case for those needing ongoing opioid therapy.

Premenopausal women who have their ovaries surgically removed face an increased risk of developing chronic kidney disease, according to a Mayo Clinic study published on Wednesday, Sept. 19, in the Clinical Journal of the American Society of Nephrology.
“This is the first study that has shown an important link between estrogen deprivation in younger women and kidney damage. Women who have their ovaries surgically removed have an increased long-term risk of chronic kidney disease,” says Walter Rocca, M.D., a Mayo Clinic neurologist and epidemiologist, and senior author.
The research team used data from the Rochester Epidemiology Project to determine these findings.

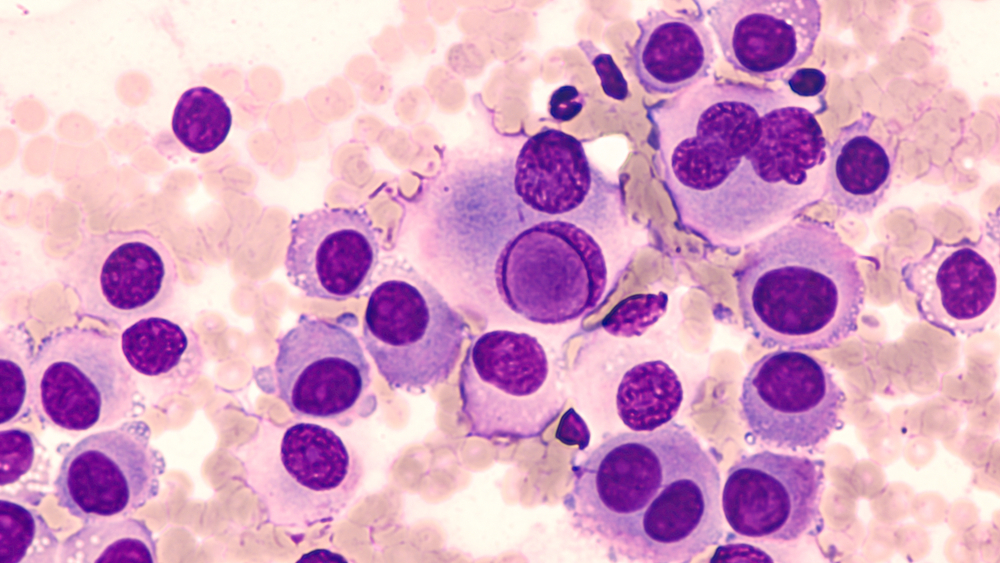
Zombie cells are the ones that can't die but are equally unable to perform the functions of a normal cell. These zombie, or senescent, cells are implicated in a number of age-related diseases. And with a new letter in Nature, Mayo Clinic researchers have expanded that list.
In a mouse model of brain disease, scientists report that senescent cells accumulate in certain brain cells prior to cognitive loss. By preventing the accumulation of these cells, they were able to diminish tau protein aggregation, neuronal death and memory loss.
Resident physician burnout in the U.S. is widespread, with the highest rates concentrated in certain specialties, according to research from Mayo Clinic, Oregon Health & Science University and collaborators. The findings appeared on Tuesday, Sept. 18, in the Journal of the American Medical Association. Physician burnout is a dangerous mix of exhaustion and depersonalization that contributes to physicians making mistakes while administering
health care.
Mayo Clinic physicians Matthew Block, M.D., Ph.D. and Tina Hieken, M.D., have received a Stand up to Cancer (SU2C) Catalyst Award to fund melanoma research and a neoadjuvant clinical trial.
“This study, “Neoactivate”, will test two novel approaches to the treatment of patients with high-risk, stage 3 melanoma guided by specific mutations within the melanoma,” says Dr. Hieken. “Two combinations of immunotherapy and targeted therapy will be given before surgery, and all patients will receive immunotherapy after surgery.”
###
Subscribe to Advancing the Science for regular updates.
________
Other Mayo Clinic medical research websites:
- Research at Mayo Clinic
- Discovery’s Edge
- Advancing the Science
- Forefront
- Mayo Clinic Center for Individualized Medicine
- Mayo Clinic Center for Innovation
- Center for Regenerative Medicine
- Center for the Science of Health Care Delivery








