-
Science Saturday: Researchers explore personalized approach to anti-obesity medications
Individualized medicine initiatives mainly focus on rare diseases or cancer. Little has been attempted to individualize treatment for noncommunicable chronic diseases such as obesity — a chronic, relapsing disease, and a primary cause of Type 2 diabetes, fatty liver disease, cardiovascular disease and cancer. There are many obesity interventions, such as diets, devices, surgery and medications. However, not much is known about the predictors of response to these obesity interventions.
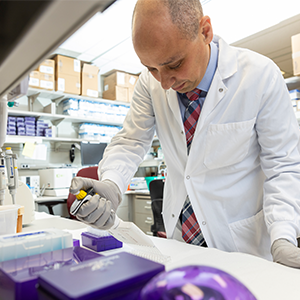
"Sustained weight loss with current treatment options remains a challenge in the clinical practice," says Andres Acosta, M.D., Ph.D., a Mayo Clinic gastroenterologist and obesity expert.
To address this, Dr. Acosta and a team of Mayo Clinic researchers set out to study anti-obesity medications based on obesity phenotypes to enhance weight loss. A phenotype is a set of observable characteristics of a person resulting from the interaction of his or her genotype with the environment.
Their findings, published in the journal Obesity, show a phenotype-guided approach was associated with 1.75-fold greater weight loss after one year and the proportion of patients who lost more than 10% at one year was 79%, compared with 34% whose treatment was not phenotype-guided.
What are phenotypes, and why do they matter?
The team stratified obesity into four phenotypes:
- Hungry brain ― mainly controlled by the brain-gut axis, and abnormal calories are needed to reach fullness.
- Emotional hunger ― desire to eat to cope with positive or negative emotions.
- Hungry gut ― abnormal duration of fullness.
- Slow burn ― decreased metabolic rate.
With regard to energy balance ― intake versus expenditure ― these four phenotypes regulate body weight.
Key drivers for intake are fullness, duration of fullness and emotional eating. Key drivers for energy expenditure are resting energy expenditure, nonexercise physical activity, exercise and the thermogenic (increase in the metabolic rate that occurs after a meal) effect of food and exercise.
"It was essential to explain differences among patients in some of these measurable components of food intake and energy expenditure, and assess their potential for individualizing therapy for obesity," says Dr. Acosta.
The team theorized that classifying phenotypes would reveal obesity subgroups and enhance response to obesity medications.
"Our aim was to characterize the obesity phenotypes and to assess the effectiveness of phenotype-guided anti-obesity medications, compared with non-phenotype-guided medication."
The Mayo team conducted a yearlong clinical trial performed in a weight management center where 312 patients were randomly assigned to phenotype-guided treatment or treatment that was not phenotype guided and included anti-obesity medications.
"Our long-term goal is to develop a personalized approach to identify the right medication for the right patient, minimizing side effects to obesity management." - Dr. Acosta
In the era of individualized medicine, the proposed phenotype-guided stratification and treatment approach, in addition to the positive outcomes reported in previous randomized trials, represent a step toward a precision medicine approach to optimize obesity therapy.
"Biological and behavioral phenotypes clarify the complexities of human obesity and can be targeted with medications to enhance weight loss," says Dr. Acosta. "Our long-term goal is to develop a personalized approach to identify the right medication for the right patient, minimizing side effects to obesity management."
Dr. Acosta's research encompasses many key areas of individualized medicine. His team applies principles of pharmacogenomics ― how drugs interact with genes ― in obesity to better understand how the disease develops, reduce treatment inconsistencies and decrease the treatments' side effects. His goal is to stratify obesity to support the development of personalized drugs to treat obesity and generate safer and more effective medications.
Dr. Acosta received the Mayo Clinic Center for Individualized Medicine Gerstner Career Development Award. This award provided partial funding for this study.
Related Articles