-
Sharing Mayo Clinic: A mother’s heart: Teamwork saves new mom, son

Every birth is a life-changing event and many new parents enjoy sharing detailed birth stories to all who will listen. Some stories are about quick labor and barely making it to the hospital in time. Others tell tales of painful back contractions or long, slow labor. It's not a competition, but if it were, the prize for most dramatic birth story might go to Julie and Kyle Janzen.
May 5 started out like any other day. Julie spent the day at work, and she was looking forward to spending the evening with Kyle at a local fire department fundraiser. She was 39 weeks pregnant, and so far, the pregnancy had been uneventful.
"Overall, it was excellent. I had no morning sickness or complications," says the 37-year-old Taylor, Wisconsin, resident. "I felt great."
Concerning symptoms
While at the fundraiser, Julie's condition suddenly changed. "My vision blurred, and I had a strong pain in my upper chest. At first, I thought I swallowed wrong," she says.
Julie and Kyle weren't sure if she was in labor, so they asked an EMT at the event to check her vitals signs. They were good, but the volunteer noticed her pupils were dilated and recommended that she be evaluated at a hospital right away.
Kyle and Julie arrived at Mayo Clinic Health System in Eau Claire and were met by Carla Williams, M.D., the OB-GYN on call.
"Julie had chest pain that wrapped around to the upper middle part of her back. We quickly determined that she was not in labor," says Dr. Williams. "We got vital signs on her right away. They were OK, but her oxygen saturation level would drop when she took a few steps."
Dr. Williams' first concern was that Julie had a blood clot in her lungs, but the CT scan for pulmonary embolism was negative. Julie's pain continued, and her oxygen levels and baby's vital signs were fluctuating, so she was moved to the Critical Care Unit.
During this time, Julie remained alert and talking with the staff. However, when reflecting on it, she says, "They said I was coherent and answering questions, but I don't remember any of it."
Unlike Julie, Kyle's memory of these anxious hours is clear. With Julie awake and appearing normal, he relied on her judgment for key decisions. "I was ready to overrule her if necessary, but she made all the right calls," he says.
Life-threatening diagnosis
When she arrived in the Critical Care Unit, the team ordered an echocardiogram to evaluate her heart and blood vessels.
"The echocardiogram was ordered because fetal heart tracing indicated that the baby was not doing well and wasn't tolerating whatever was going on," says Dr. Williams. "The baby's vital signs, specifically the fetal heart rate pattern, were a significant indicator that mom's status was not stable, even though her own vital signs looked OK while she was at rest."
The echocardiogram revealed what was the cause of Julie's pain: a life-threatening aortic dissection.
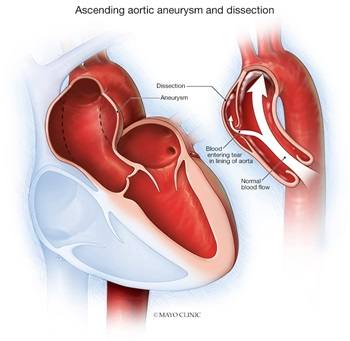
"An aortic dissection is an extremely dangerous acute event with high fatality rates," says Nishant Saran, M.B.B.S., a cardiovascular surgeon. "The aorta, which is a tube that carries the blood away from the heart to the rest of the body, develops a tear and the blood seeps into the layers of the aorta, creating a false channel. Often, this compromises the blood flow in the true channel leading to organ failure or stroke from lack of effective blood supply to the organs and brain. There is also a huge risk that the aorta itself may rupture, leading to almost instant death."
A team, including Cardiovascular Surgery, Cardiology, Neonatology, Obstetrics and Anesthesia providers, was quickly convened to develop a plan to save two lives: Julie and her baby.
"With this condition, about 80% of people never make it to the hospital," says Robert Wiechmann, M.D., a Mayo Clinic Health System cardiovascular surgeon. "For the rest, every hour that passes, the risk of death goes up 10%. We needed to act immediately."
"Aortic aneurysms in pregnancy are incredibly rare but often fatal," says Dr. Williams. "This is because of the physical changes in pregnancy, which are most pronounced in the third trimester ― like Julie."
Only about 0.05 per 100,000 women develop an aortic aneurysm or dissection during pregnancy. In women with a known aortic aneurysm, they have a 25 times higher risk of dissection during pregnancy, explains Dr. Williams.
Surgical plan
The team explained to Julie and Kyle that two surgeries would be needed: one to deliver their child and a second to repair her aorta.
"When the doctor told us what was going on, my heart just dropped," says Kyle. "Julie was a true champ. She kept saying, 'We've got this.' She was so strong."
A big challenge would be to balance the risk of bleeding versus developing blood clots. During routine heart surgeries, patients are given anticoagulation medications to thin the blood and prevent clots. However, this wasn't possible for Julie because of the risk of blood loss following a cesarean section.
Another challenge was the complex task of keeping Julie properly anesthetized during her surgeries and her blood pressure steady ― all while minimizing sedation effects on the baby. Westley Manske, D.O., a Mayo Clinic Health System anesthesiologist, explains that a woman's cardiac output increases naturally after delivery. This change can affect her blood pressure and pressure on the aorta that increases her risk of rupture.
"Blood pressure management was critical to preventing worsening of the dissection or rupture. Normally, the goal would be to lower her blood pressure, but since she was pregnant, lowering it too far could be dangerous for the baby who might need a higher pressure for enough placental blood flow," says Dr. Manske. "We choose a special opiate medication not normally used for this type of surgery that helped with her blood pressure and rapidly wore off so the baby would not experience any adverse effects from a longer-acting opiate medication."
C-section delivery
In the morning hours of May 6, Julie was wheeled into an operating room while Kyle waited for the birth of their child, and to learn about the health and safety of his wife.
Dr. Manske administered the anesthetic, and Dr. Williams performed an emergency C-section to safely deliver Julie and Kyle's son, Logan. He weighed 8 pounds, 14 ounces. He was quickly transferred to the Level 2 Special Care Nursery to meet his dad for the first time.
"Everyone gave a sigh of relief to hear the baby cry," says Mark Twesme, a cardiovascular surgery physician assistant. "Immediately following that, we began the heart surgery and focused completely on Mrs. Janzen's heart condition and the repair."
Julie's C-section incision was left partially open so the team could monitor her for bleeding that could develop during her heart procedure.
Aortic dissection repair
During the 12-hour heart surgery, Drs. Wiechmann and Saran worked together to remove the section of Julie's dissected aorta and replace it with a synthetic tube, called a graft.
The first step was to connect Julie to a cardiopulmonary bypass machine that replaces the heart's pumping action and adds oxygen to the blood during surgery. Then they began cooling Julie's body, allowing surgeons to stop her heart and make the necessary repairs without damaging heart tissue.
"Once we reached the temperature of around 18 degrees C or 64 degrees F, we stopped all circulation and removed the dissected aorta, and replaced it with the graft, reestablishing blood flow to the brain and other organs," says Dr. Saran.
During the procedure, the surgical team discovered that Julie had additional damage to other vessels and the aortic valve in her heart.
"Our job was to reestablish the true channel and then fix whatever else is damaged. In Julie's case, the aorta was torn all the way down to the aortic valve and she had tears into the major vessels going to the right arm and brain. All of this needed to be reconstructed," says Dr. Wiechmann. "It was very challenging. There is no routine dissection repair surgery, since each one is different. In these cases, surgeons have to take their skill sets and adapt them to the unique situation."
While Julie was in surgery, Kyle was caring for Logan in the Level 2 Special Care Nursery, which is part of the Family Birth Center.
"I was nervous, but the nurses there helped me out immensely. They showed me how to change diapers, feed him and answered every question I had," recalls Kyle. "I knew what Julie wanted, so I did skin-to-skin contact right away and requested donor milk for Logan, too."
That evening, the Cardiovascular Surgery team completed the necessary repairs, Julie's incisions were fully closed, and she was transferred to the Critical Care Unit for recovery. It wasn't long before she had a young visitor, who brought with him Mother's Day cards made by nurses in the nursery.
"I wasn't able to see Logan upstairs, but they brought him down to me the same day that I woke up," says Julie. "They did his first bath in my room, and we were able to do skin-to-skin as soon as they removed my ventilator."
Two setbacks
The new family recovered and got acquainted over the next four days. However, they experienced two setbacks on May 10. Logan struggled to maintain his oxygen level, and he was transferred to Mayo Clinic Hospital ― Rochester in Rochester, Minnesota, for additional testing and monitoring. Soon after, he was discharged home with Kyle.
Back in Eau Claire, Julie experienced some internal bleeding on her heart. During many heart surgeries, temporary pacing wires are applied to the heart and connected to an external pacemaker. These wires are removed at the bedside a few days after surgery. For Julie, removing one of the wires caused bleeding, and she needed to have another surgery to solve the issue.
Julie put on a brave face for Kyle. "He was so worried and panicked. I kept telling him, 'We've got this,'" she says. "I tried to be cheery the whole time because I was determined to go home. I had a newborn waiting for me."
Right before this second surgery, Julie's cheerful demeaner needed a bit of extra comfort and support. "Mark (Twesme) calmed me down before my second surgery," says Julie. "He held my hand and told me that everything would be fine."
"I could see it on her face that she was extremely scared after just a few days earlier going through a life-threatening surgery. To now have another problem that could be life-threatening was scary," says Twesme. "My job at that time was to just provide support in any possible way."
Twesme was right, and Julie's second procedure went well. Drs. Saran and Wiechmann, with anesthesia administered by Dr. Manske, discovered that a small clip next to the vein graft was dislodged when the pacing wire was removed. They applied another clip, and her bleeding was controlled.
The rest of her recovery was uneventful, and Julie was able to go home to Kyle and Logan on May 16.
Recovery at home
Once home, Julie was determined to get stronger and be able to care for Logan.
"I did all my cardiac rehab at home because of having Logan," says Julie. "I have a pedal (stationary) bike and breathing machine that I used every day. I told myself that I wouldn't get better if I didn't."
Soon she was back on her feet and adjusting to motherhood. Julie reports that she was feeling so well that she was able to return to work full time just 12½ weeks after Logan's birth and her two heart surgeries.
After his dramatic entrance into the world, Logan is settling in and charming his family and friends.
"He's perfect. We couldn't ask for anything better," says Kyle. "Everyone says he looks like me. He has Julie's fingers and toes, but everything else is pretty much dad."
"He just started rolling over, and he's not fussy at all," says Julie. "He is just a blessing from God."
When reflecting on Logan's birth, the couple is amazed. "I can't believe we went through all of this, but everything is turning out OK," says Kyle.
"Even today, I can't believe everything that happened," says Julie. "The medical staff ― the entire team ― all were phenomenal. They did an amazing job."
And Julie's care team in Eau Claire couldn't be more pleased.
"This really highlighted the collaborative care with Mrs. Janzen and her baby at the center of every decision made," says Twesme. "It really demonstrated that the needs of the patient always come first."
"I'm incredibly blown away by the teamwork," says Dr. Williams. "I'm so grateful that we had this amazing team to save her life and the baby's life."
Dr. Wiechmann agrees. "No matter what we do, it takes a team," he says. "Everything we do, we have a large group of people that work together, care about each other and do great work. It's an amazing place."
This story also appears on the Mayo Clinic Health System Hometown Health blog. You can find it there and share it with others https://www.mayoclinichealthsystem.org/hometown-health/patient-stories







